- solen.cz - Genetic haemochromatosis, one cause, multiple diseases. Solen. Bedrich Stanka, MD and co.
- casopisvnitrnilekarstvi.cz - Molecular genetic diagnosis and screening of hereditary haemochromatosis. Journal of internal medicine. J. Zloch et al.
- medlineplus.gov - Hereditary hemochromatosis. Medline Plus - National Library of Medicine
- healthline.com - Hemochromatosis. Healthline - Health and Health. April Kahn
Hemochromatosis and iron problem? Why does it occur and what are the symptoms?
Hemochromatosis refers to a disorder of excessive iron absorption in the human body. How does this disease arise and what are its first symptoms?
Most common symptoms
- Malaise
- Loss of pubic hair
- Breast enlargement in men - Gynecomastia
- Abdominal Pain
- Joint Pain
- Frequent urination
- Spirituality
- Hyperpigmentation
- Bleeding
- Swelling of the limbs
- The Island
- Erectile dysfunction
- Bone thinning
- Muscle weakness
- Fatigue
- Water in the abdomen
- Decrease in libido
- Liver enlargement
- Increased blood sugar levels
- Increased iron levels in the blood
Characteristics
Hemochromatosis can arise on a genetic basis, but also due to the presence of other diseases in the body. In an individual, there is an increased absorption (in the small intestine) and deposition of iron.
You can learn about the exact etiology, manifestations, prognosis, treatment options and much more in the article.
What is hemochromatosis?
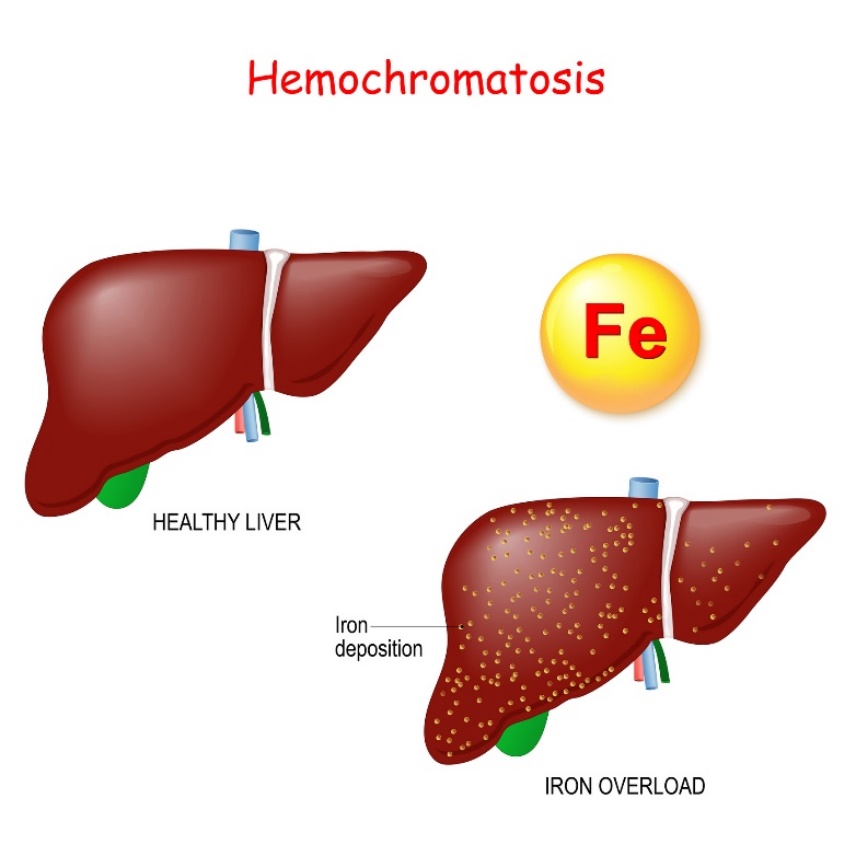
Haemochromatosis is a disease caused by increased resorption of iron from the digestive tract and its excessive deposition in the organ parenchyma (organ tissue).
The concentration of iron in the body can gradually reach more than ten times the original physiological value.
Under physiological conditions, approximately 4-5 g of iron is present in the human body.
Of the total amount of storage iron, 40% is stored in the liver,
mainly in hepatocytes (liver cells).
Haemochromatosis is divided according to the aetiology of its onset into primary (hereditary genetic) and secondary (iron accumulation due to another disorder).
Genetic hemochromatosis (GH), also referred to as hereditary, is a common autosomal recessive inherited disorder. Its basis is excessive iron deposition in the body.
Increased iron absorption in the organs leads to their progressive change and damage. The disease was first described by Dr. Troiser in 1871.
The disease manifests slowly and gradually and the individual may not be aware of the increased iron deposition for several decades.
Most often, the first thing noticed is elevated blood iron levels. Later, elevated blood sugar, an enlarged liver and specific hyperpigmentation of the skin will appear.
Secondary haemochromatosis can also occur as a result of other diseases such as anaemia, diabetes, alcoholism, kidney dialysis and last but not least chronic liver disease.
Various health risks and associated complications arise in haemochromatosis. Most of these arise in organs that store excessive amounts of ingested iron.
The damage occurs gradually and continuously over time. The resulting changes mainly affect the liver, pancreas, heart and skin.
Advanced haemochromatosis can result in liver damage which can cause cirrhosis (chronic liver scarring). Damage to the pancreas can in turn cause changes in insulin levels with a risk of diabetes.
Blood circulation problems can lead to cardiovascular failure or heart failure. Iron deposition in the heart can also cause irregular heart rhythms (arrhythmias) or cardiomyopathy.
Excessive iron in the body can cause hyperpigmentation. The skin may appear bronzed to gray.
Causes
The most common cause of haemochromatosis is a mutation in the HFE (High Iron Fe) gene. The HFE gene is responsible for making a protein that regulates the absorption of iron from the diet.
The HFE gene mutation is present in approximately 80% of patients with primary (genetic) haemochromatosis.
The disease caused by the HFE gene is the most common and is therefore referred to in the literature as genetic haemochromatosis type 1.
GH is caused by mutations in the HFE gene on chromosome 6. The most common mutation is C282Y, which has the most severe course of the disease.
A person must inherit a copy of the pathological gene from each parent to fully transmit the diagnosis. If a person inherits only one copy of the mutated gene, they are considered to be a carrier of haemochromatosis and may never develop it.
Symptoms
Haemochromatosis is a long, asymptomatic disease that in most cases does not become apparent until around the age of 30 or 40.
In particular, there is chronic remodelling of liver tissue and possible development of cirrhosis. Hepatomegaly - enlargement of the liver - is also a symptom.
Increased grey-bronze pigmentation of the skin, increased weakness, fatigue, abdominal pain and also weight loss are characteristic.
Hemochromatosis is also called bronze diabetes.
Bronze diabetes is caused by destruction of the islets of Langerhans of the pancreatic organ and consequent inability to produce insulin.
It is characterized by the associated occurrence of diabetes mellitus (diabetes), cardiomyopathy, arrhythmia, arthropathy and other disorders due to elevated iron and blood sugar levels.
Joint disorders and degeneration, muscle weakness and thinning of the bones often occur.
Frequent manifestations of haemochromatosis:
- Bronze (grey) hyperpigmentation of the skin
- Enlargement of the liver (hepatomegaly).
- Cardiovascular disorders
- Cardiac arrhythmias
- Diabetes mellitus (diabetes)
- Joint and muscle weakness
- Abdominal pain
- Weight loss
Diagnostics
The basis of the diagnosis of haemochromatosis is the determination of an elevated iron concentration in the blood by means of a blood test. The result is evaluated by means of special tests for iron and ferritin levels in the blood serum.
GH is characterised by an increase in transferrin iron saturation above 55% and an increase in ferritin above 500 µg/l.
In advanced stages of haemochromatosis, serum ferritin concentrations are usually above 1000 ng/ml.
A reliable test is the determination of the iron concentration in the dry liver. It is accurately expressed by the liver iron index.
An elevated ferritin concentration must be distinguished in the context of a possible inflammatory process, tumour, liver disorder or alcoholism of the patient.
The standard in the diagnosis of haemochromatosis is primarily genetic testing. DNA testing is based on the examination of mutations in the HFE genes. The three most common mutations in haemochromatosis are determined.
Currently, the C282Y and H63D mutations in the HFE gene should be determined in every patient with genetic haemochromatosis. The test is currently available in specialised medical centres.
CT scanning mainly detects the accumulation of iron in the liver in hyperdense livers. Magnetic resonance imaging can determine the presence of iron in the liver. It is useful for quantitative estimation of iron in the liver.
The physiological value of liver iron content determined by MRI is less than 36 µmol/g. In contrast, values higher than 85 µmol/g are typical of haemochromatosis.
As the liver is the primary iron storage organ, a liver biopsy is also performed. In a liver biopsy, a small portion of liver tissue is removed and examined for the presence of organ damage.
Prognosis of haemochromatosis
An early diagnosis of haemochromatosis and its subsequent expert treatment has an excellent prognosis. With the right lifestyle, treatment and the right procedures, the patient can manage the clinical symptoms and the disease itself and live a full life.
However, with advanced organ damage due to excessive iron deposition, a very good prognosis cannot be expected.
Untreated patients with genetic haemochromatosis most often die of severe liver cirrhosis, hepatocellular carcinoma, diabetes mellitus or cardiomyopathy.
How it is treated: Haemochromatosis
Treatment of haemochromatosis: Drugs? Diet and lifestyle
Show moreHaemochromatosis is treated by
Interesting resources










