- solen.sk - Current views on the issue of mild brain injury
- neurologiepropraxi.cz - CURRENT NEUROSURGICAL APPROACHES TO CONCLUSIVE HEAD INJURIES
- fmed.uniba.sk - Selected chapters from pediatric surgery
Concussion: what is it and what are the symptoms?

A concussion (commotio cerebri) is a transient disturbance of brain function. It is caused by external forces. It is referred to as a mild brain injury.
Most common symptoms
- Malaise
- Headache
- Sensitivity to light
- Depression - depressed mood
- Sweating
- Nausea
- Low blood pressure
- Concentration disorders
- Memory disorders
- Disorders of consciousness
- Mood disorders
- Muscle weakness
- Head spinning
- Fatigue
- Anxiety
- Vomiting
- Confusion
- Accelerated heart rate
Characteristics
The now-famous term "concussion" was first used by the famous Arab physician and philosopher Razi Abu Bakr Muhammed ibn Zakariya, known in Europe as Rhazes. It was he who described concussion as a functional brain disorder without obvious traumatic damage.
This was a watershed moment for medicine at the time and is the basis for our understanding of the disorder today.
The modern technical term for concussion is mild brain injury. It belongs to the group of so-called diffuse axonal injuries.
It accounts for 70-90% of all head and brain injuries.
Worldwide, it occurs in 600 people per 100 000 population per year. Approximately half of them require hospitalisation. Men are affected twice as often as women. The most at risk group is young people aged 15 to 24.
Concussion is a reversible and global disorder of brain function.
It is a transient loss of function of synapses, which are connections between individual nerve cells. Synapses are used to communicate between nerve cells and to transmit information to higher or lower brain centres. In concussion, there is a generalised asynapse, or momentary loss of nerve connections.
It is caused by an external mechanical force. Most often it is a direct blow to the head, face, neck or other part of the body with transmission of inertial forces to the cranial cavity where the brain is located.
Damage to axons results in sudden changes in neurological function. These changes are caused by functional loss of some neuronal connections rather than structural damage.
Structural damage to the brain does not occur.
Concussion manifests itself in characteristic subjective and objective symptoms. The symptoms are not permanent, they occur only transiently. Their resolution is usually gradual. Some injured persons may suffer symptoms for a longer period of time.
The difficulties are not permanent.
Causes
The basic cause is a sharp acceleration or deceleration of the head.
With such a sudden change in the movement of the head, the position of adjacent parts of the brain changes. These individual parts of the brain shift due to inertial force and the fine nerve fibres - the axons - are disrupted.
This damage occurs in the white matter of the brain.
The reticulocortical pathways are most affected. These pathways connect the brain stem, specifically the reticular formation, to the cerebral cortex. The disconnection of these two functional units results in the most typical symptom of concussion, i.e. unconsciousness.
If the axonal damage is not extensive, only a change in consciousness may occur. The change in consciousness is manifested by various disturbances in the perception of the environment.
Axonal damage is caused by two mechanisms:
- Axon stretch - This damage is reversible, i.e. reversible. Nerve connections can still regenerate to their original form.
- Axon rupture - This damage is irreversible, i.e. permanent.
The most common causes of concussion:
- Car accident.
- Gunshot wounds
- pedestrian collision
- work accidents
- sports injuries, e.g. cycling, skiing, skating
- falls from stairs, ladders, beds and trees
- assault

In these accidents, there is a specific mechanics to the injury. It can be a head movement that is suddenly stopped by an immovable object, such as a head hitting a windshield in a car accident, a head fall that hits the ground, etc.
The second mechanism of injury is the forceful impact of a moving object on the head, such as a blow from a blunt object in a violent assault.
Symptoms
The clinical picture of concussion must meet at least one of the following features:
- confusion or disorientation
- unconsciousness lasting less than 30 minutes (may not occur at all)
- post-traumatic memory loss, called amnesia, which lasts no more than 24 hours (usually the patient has no memory of what happened to him or of the injury or its circumstances)
- other focal neurological symptomatology, such as neurological deficit or the presence of convulsions
Consciousness and its disturbances
The most dramatic symptom of concussion may or may not be short-term unconsciousness.
Alterations of consciousness, such as memory impairment, disorientation in space and time, confusion, and behavioral changes, are more often present than complete unconsciousness.
Examples of characteristic behavioural changes are as follows:
- Slowed reactions
- repetition of the same questions
- talking nonsensically
- impaired coordination of movements
- restlessness
- emotional instability
- anxiety
- tearfulness
These symptoms usually disappear within a few minutes.
Deterioration of memory
Memory impairment can be divided into two types based on the temporal sequence of amnesia:
- Retrograde (pretraumatic) amnesia - The injured person has no memory of the circumstances of the injury and what preceded it, no recollection of the time before the injury.
- Anterograde (post-traumatic) amnesia - No memory of the events after the accident, no memory of where he woke up, what happened to him after he woke up, etc.
Spasmodic activity
These are coma spasms that are not part of the seizure set. They occur about 2 seconds after a blow or impact.
The onset of convulsions is characterised by the injured person briefly becoming completely rigid, followed by bilateral but asymmetrical twitching of the upper and lower limb muscles. They may last up to 3 minutes.
They are similar in character to the so-called spasmodic syncope.
Somatic accompanying symptoms
A few minutes after the concussion, symptoms begin to come to the forefront of the clinical picture, which the injured person may suffer for varying lengths of time.
These symptoms include:
- headache
- dizziness
- nausea
- vomiting
- insomnia
- rapid fatigue
- hypersensitivity to light and noise
- attention disorders
- memory disorders
- slowing of thinking
- reduced performance
- emotional instability
- depressed mood
- anxiety
- nervousness
- apathy
Some of these do not appear until 1-2 weeks after the injury.
Symptoms tend to severely limit the patient's ability to integrate into normal personal and professional life.
Diagnostics
Diagnosis is based on a history of head trauma with characteristic mechanics. In addition, a neurological examination or examination by a traumatologist is beneficial.
The neurologist looks for focal symptomatology. He checks pupillary movements, eye movements, sensitivity, tendon-muscle reflexes, pyramidal phenomena, meningeal symptoms and others.
The Glasgow Coma Scale (GCS) was developed by experts for objective assessment of consciousness.
It assesses disturbances in three neurological categories:
- eye opening - 1 to 4 points
- spontaneous eye opening (4 points)
- opening on address (3 points)
- opening on painful action (2 points)
- no eye opening (1 point)
- best vocal expression - 1 to 5 points
- appropriate verbal response (5 points)
- inadequate verbal response (4 points)
- responds only with single words (3 points)
- unintelligible sounds (2 points)
- no answer (1 point)
- best motor response - 1 to 6 points
- performs an appropriate movement when prompted (6 points)
- performs an automatic defensive movement to a painful stimulus (5 points)
- performs an automatic escape movement to a painful stimulus (4 points)
- perform a non-specific limb flexion movement to a painful stimulus (3 points)
- perform a non-specific limb extension movement to a painful stimulus (2 points)
- no movement in response to pain (1 point)
If the sum of GCS scores is 15-13, no or only mild impairment of consciousness is present.
If the GCS score is 12-9, there is moderate impairment of consciousness.
A GCS less than 8 indicates severe impairment of consciousness and coma.
The trauma surgeon attends to obvious external injuries to the hard covers of the head or other injuries resulting from more extensive polytrauma.

The next step in assessing which brain disorder is involved is to perform an imaging study. The most readily available and quickest to perform is a CT scan of the brain. Its findings are negative for concussion, and the brain tissue is free of obvious structural changes.
Magnetic resonance imaging of the brain, however, can show changes in the signal of the tissue. These are characteristically luminous (hypersignal) foci in the corpus callosum (part of the brain belonging to the so-called basal ganglia), in the white matter of the test under the cerebral cortex, in the thalamus and in the brain stem.
Differential diagnosis
For a correct diagnosis, it is important to exclude other causes of unconsciousness:
- epileptic seizure
- syncope (short-term unconsciousness with sudden drop in blood pressure)
- cardiac arrhythmia
- intoxication (poisoning)
- decompensation of diabetes and subsequent coma
Routine investigations such as blood draw for biochemical tests, blood count, ECG, X-ray and others follow.
Course
After a strong blow or impact, there is a short-term "shutdown". Often unconsciousness occurs, but this is not a condition. Hypotonia (reduced muscle tone), loss of tendon-muscle reflexes, slowed heart rate (bradycardia), reduced blood pressure (hypotension) are present.
Gradually, the injured person regains consciousness.
Immediately on waking, he is disoriented. He cannot recognise where he is, what day it is, what has happened to him. He is unaware of his other injuries.
He is unable to perform simple tasks and commands, cannot stand up, is slow, speaks incoherently, often unconsciously. His movements in carrying out normal activities are uncoordinated.
Such a situation worries the patient.
There is anxiety, shock, crying and depressive thoughts.
Some specific types of people experience concussion with characteristic differences. This group includes people who have already had some functional and structural damage to the brain before the injury. These include alcoholics, substance abusers, people with degenerative brain disease and others.
They wake up from unconsciousness restless, aggressive, rejecting the reality and severity of the injury. They often want to leave the first aid facility, pushing away the attending persons. This condition is called post-traumatic somnolence.
Symptoms after concussion
Symptoms usually subside within a few days or weeks.
Peak athletes suffer symptoms after a concussion for 7 to 10 days. The general population of people describes the disappearance of subjective complaints within 3 to 12 months.
Approximately 5% of patients who have sustained a concussion continue to suffer at least one symptom for a year after the injury.
The most common symptoms are:
- headache
- dizziness when changing the position of the head or body
- fatigue
- disturbances in attention
- memory disorders
Repeated head injuries, such as in boxers, that are accompanied by concussion can lead to a neurodegenerative disease called progressive tauopathy. This is also referred to as chronic traumatic encephalopathy.
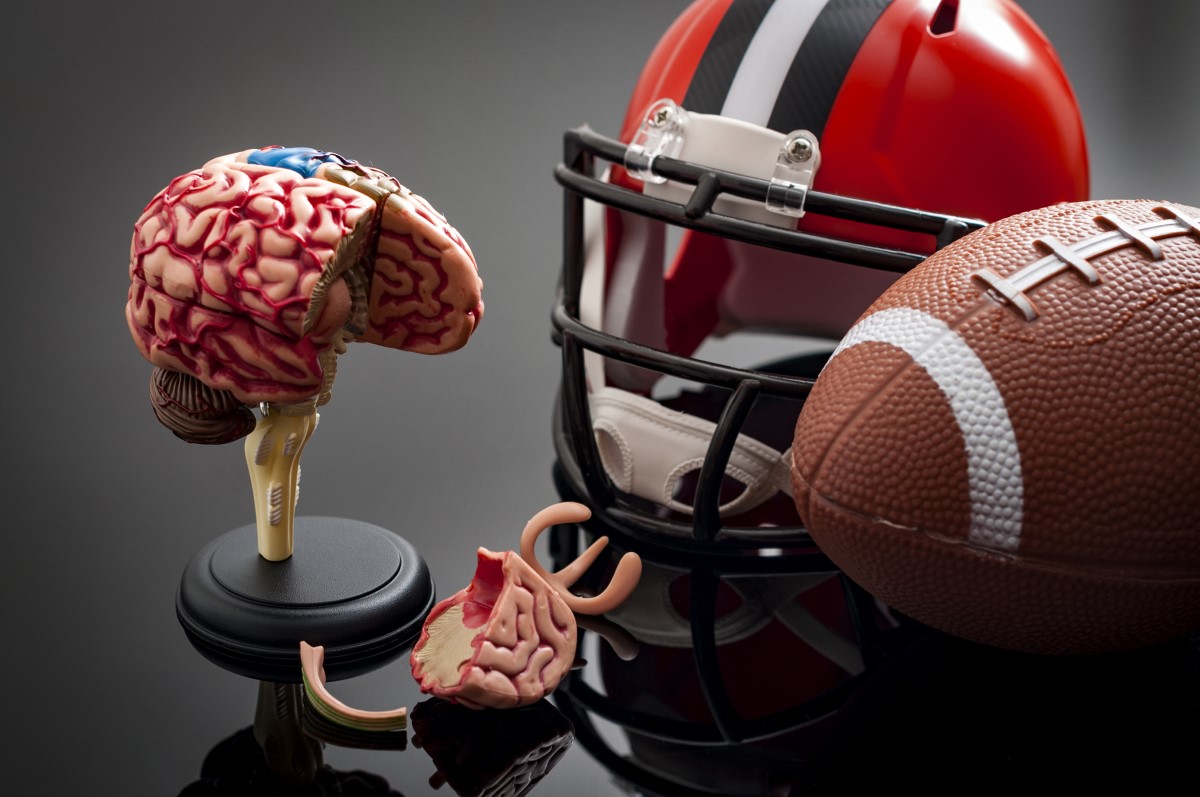
Athletes under the age of 20 who are exposed to repeated concussions can develop a dreaded disease called second impact syndrome.
It causes swelling of the brain after a second concussion at a time when the patient has not yet recovered from the first concussion.
As a result of repeated trauma, the blood vessels suddenly lose their ability to regulate their blood pressure with a concomitant increase in pressure caused by released adrenaline and stress.
This syndrome has up to a 50% mortality rate.
Concussion in childhood
In children, this is the most common type of craniocerebral injury overall.
As in adults, it is a diffuse and functional injury that is fully reversible.
Unconsciousness is not a condition in children either, but it can occur, and at varying depths.
The clinical picture bears the following features:
- unconsciousness
- amnesia
- nausea
- vomiting
- headache
- confusion
- dizziness
- drowsiness
- disturbances in concentration
- double vision
- nervousness
- slowed reactions
- stability disorders
- convulsions
A combination of several symptoms is common.
The most serious are unconsciousness, vomiting and amnesia.
Memory impairment is most often retrograde. That is, the child has no memory of the circumstances immediately before the accident.
Diagnosis is based on history and neurological examination. In severe head injury, examination by a trauma surgeon or surgeon is necessary.
Among imaging examinations, CT and MRI of the brain are the most important. Ultrasonography (USG) of the brain through the fontanelle is also possible in children who have not yet fused the cranial sutures.
The treatment process begins with observation of the patient. In the home environment, physical rest, adequate sleep and consistent hydration are ordered. In young children with constant vomiting, infusion rehydration therapy is necessary.
Read also the article:
How to recognize a concussion in children? How does it manifest and why be alert?
How it is treated: Concussion
How is concussion treated? Observation as number 1
Show moreHow a concussion occurs and how it manifests itself - video
Concussion is treated by
Concussion is examined by
Other names
Interesting resources










