- neurologiepropraxi.cz - Acute infections of the central nervous system
- solen.sk - Bearing intracranial processes of infectious etiology, Petr Kaňovský a spol. (2020), Special Neurology, Volume I, Infectious diseases of the nervous system
Brain abscess: what is it and how does it manifest itself? Why does a brain infection occur?

An abscess is a pus-filled cavity in the tissue. It manifests as a circumscribed and encapsulated inflammation. The most common bacteria that form abscesses are staphylococci and streptococci.
Most common symptoms
- Malaise
- Speech disorders
- Headache
- Sensitivity to light
- Increased body temperature
- Nausea
- Head spinning
- Double vision
- Fever
- Tinnitus
- Blindness in one eye
- Falling eyelids
- Concentration disorders
- Disorders of consciousness
- Mood disorders
- Slowed heartbeat
- Muscle cramps
- Fatigue
- High blood pressure
- Confusion
- Accelerated heart rate
- Vomiting
Characteristics
An abscess is a cavity in the tissue of the body that is filled with pus. It is an infectious disease that manifests itself in a circumscribed and encapsulated inflammation.
Certain types of bacteria, fungi and parasites are characterized by their ability to form abscesses. The most common bacteria that form abscesses are staphylococci and streptococci.
Pus is a yellow-green, thick, cloudy fluid that is formed by the accumulation of dead bacteria, live bacteria, dead white blood cells and tissue debris.
The formation of an abscess indicates the inability of the body to destroy the infection, but at the same time, the body is able to at least contain the inflammation. Therefore, abscesses form especially in patients with compromised immunity, especially its cellular component.
Brain abscess belongs to the focal intracranial infections.
The infectious focus is located in the brain tissue, where inflammation directly destroys the brain parenchyma. The surrounding tissue responds to the inflammation and oppression by forming a large swelling (edema) of the brain.
It is now a relatively rare disease.
In developing countries, however, it is twice as common, with a high risk of death. In general, brain abscess has a mortality rate of 0-25%. It depends on the type of infectious pathogen, the immunity of the organism and the timeliness of diagnosis.
Causes
The most common cause of brain abscess is transmission of infection from a nearby site of inflammation. Typical primary sites are otitis media, mastoid sinusitis and sinusitis.
A less common source of inflammation is an abscess in the oral cavity, e.g. in the case of disease or inflammation of the teeth and gums.
If the inflammation penetrates from the middle ear and mastoid sinuses, the abscess will be located in the temporal lobe.
If inflammation occurs in the frontal and olfactory sinuses, an abscess may form in the frontal lobe. Penetration from the paranasal sinuses will produce an abscess in the pituitary region.
Another possibility is transmission by blood (haematogenous route) from a distant inflammatory focus. Such a focus may be a suppurative process in the lungs or infective endocarditis (inflammation of the inner lining of the heart and valves).
The most typical bacterial, parasitic and mycotic agents are:
- Streptococcus
- Staphylococci, especially Staphylococcus aureus
- Enterococci
- Enterobacteriaceae
- Pseudomonas
- Haemophillus
- Actinomycetes
- Toxoplasma gondii parasite
- from fungi especially Candida and Aspergilus
Immunocompromised people are most susceptible to abscess formation.
These are patients with malignant disease, such as haemato-oncology, HIV positive patients, people treated with corticosteroids, after tissue transplantation, with diabetes, with neutropenia (low neutrophil count, the cells that effectively fight bacteria), with extensive burns, long-term broad-spectrum antibiotic treatment or premature newborns or children with congenital, for example heart defects.
A specific group of patients are travellers who come from endemic areas of the world that are infested with parasites. The cause of abscess in this population is tapeworm larvae, amoebae, flukes and others.
Infection occurs through ingestion of infected water or undercooked meat.

Symptoms
The clinical picture includes general symptoms from the present neuroinfection:
- 70-80% report headache
- elevated temperature, especially in the early stages when the abscess is not yet completely encapsulated
- nausea
- vomiting
- stiff neck
- epileptic seizure
- disturbances of consciousness
- confusion
- paralysis of limbs or facial nerves
Certain specific pathogens produce other typical symptoms.
An example is cerebral aspergillosis, in which small blood clots form in the blood vessels of the brain, so that the clinical picture resembles a sudden stroke. In this case, neither fever nor meningeal irritation is present.
Toxoplasmosis of the brain is characterised by extrapyramidal symptoms reminiscent of Parkinson's disease. These symptoms include various involuntary movements, trembling of the limbs, rigidity, slow movements, sluggish facial expressions, slow and silent speech and others.
In HIV and AIDS positive patients, symptoms may be initially vague and creeping. They include gradually increasing headache, with changes in personality, behaviour, disinterest, sleepiness, fever and weight loss.
Diagnostics
Diagnosis is based on a clinical picture consisting of a triad of symptoms - fever, headache and neurological deficit.
If immunodeficiency is present, this triad may not be fully expressed. The diagnosis is confirmed by imaging, which is essential in the diagnosis of brain abscess.
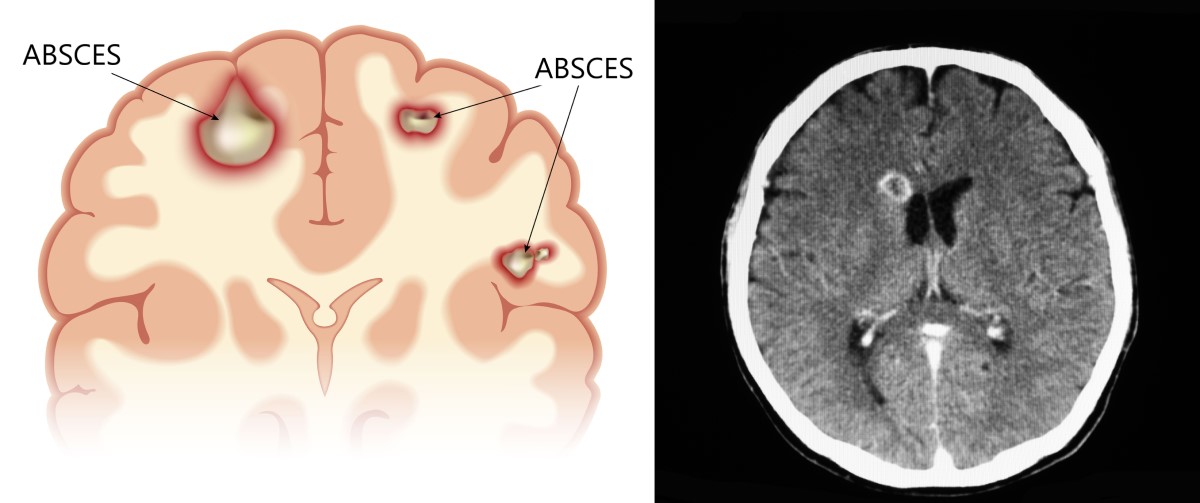
A CT scan of the brain with application of iodine contrast medium is useful. The abscess appears as a round dark lesion with a luminous ring. In the first stage (cerebritis) the ring around the abscess may not yet be visible.
The presence of cerebral oedema will appear as extensive darkening of the brain tissue. If it is at a more advanced stage, it causes oppression of surrounding structures and may push away important brain centres and ventricles, which shrink.
Magnetic resonance imaging (MRI) of the brain gives a more accurate view of the abscess. It can better differentiate between the different stages of the abscess, which may not be visible on CT. It also gives a good view of the brain oedema.
An option for advanced diagnosis is puncture of the inflamed lesion. Targeted stereotactic aspiration of the abscess is used, in which a sample of pus is taken. After microbiological analysis, the bacterial agent present in the abscess is evaluated. Antibiotic treatment can then be directly targeted to this inflammatory agent.
Lumbar puncture to remove cerebrospinal fluid is contraindicated in this case. It is therefore inappropriate. Intracranial pressure is increased in the cranial cavity by the presence of an abscess and swelling. In this case, there is a risk of herniation (dislocation) of the cerebellar parts through the inferior cranial opening during lumbar puncture. Such a complication can be fatal.
In the differential diagnosis, the most important thing is to exclude other expansive processes taking place in the cranial cavity.
Brain tumor, such as glioblastoma, or metastatic spread from a primary cancer, toxoplasmosis, subdural hematoma (bleeding under the dura), or cerebral hemorrhage come into consideration.
Course
Initially, a localised inflammation of the brain tissue - cerebritis - takes place at the site of the future abscess.
Over a period of days to weeks, the brain cells in the centre of this local inflammation gradually die. The death (necrosis) causes the solid tissue to turn into a liquid mass. This process is called collapse.
Immune cells in the brain, astroglia and fibroblasts, respond to this change by clustering and accumulating around the inflammation and necrosis. These cells confine the inflammation and form a membrane around the lesion, which can be several millimetres thick.
This is how a mature abscess is formed.
Inside the abscess, there is a fluid content consisting of dead brain cells, bacteria and white blood cells.
The course of the clinical picture can vary from mild symptoms to a dramatic infection with high temperatures and severe neurological findings.
These variations in course are due to the fact that immunocompromised patients do not respond classically to inflammation. Even with extensive infection, they may not have an elevated temperature.
However, even healthy individuals may not have a fully expressed inflammatory syndrome in cases where the abscess is well circumscribed and separated from the surrounding tissue.
Other suppurative processes in the skull
Any infectious, inflammatory and expansive process inside the skull is dangerous in terms of the development of a severe neurological clinical picture.
Subdural empyema
This is a purulent process of the mantle that insists on the brain. The pus is accumulated between the dura mater and the arachnoid. In this space between them, there is a sparse connective tissue that allows the infection to spread over large areas and considerable distance.
In about half of the patients, the transmission of infection is from suppurative sinusitis, especially from the frontal sinus, middle ear or mastoid process.
Rarely, it may occur as a complication of trauma with skull injury, after neurosurgical surgery or in purulent meningitis.
The clinical picture can be twofold.
In the acute course, the patient has high fever, intense headache and signs of rapidly increasing intracranial pressure.
Present are:
- positive meningeal phenomena from meningeal irritation
- Sleepiness
- confusion
- unconsciousness to coma
- Polio
- convulsions
- balance disorders
- trembling of the limbs
- speech disorders
If subdural empyema develops after trauma or neurosurgery, the course is slower and more creeping - subacute to chronic. There can be a time lag of up to 19 days between the surgery or trauma and the onset of empyema symptoms.
Epidural abscess
Arises from the same cause and by a similar mechanism as subdural empyema, but in this case the inflammation does not cross the dura mater. It is held above the dura mater and below the skull bone. This suppurative intracranial process is more localized and less severe than subdural empyema.
Clinical symptoms are not specific. They often overlap with symptoms of acute sinusitis or otitis (sinusitis and otitis media).
The most typical symptom is a headache, but this does not at first indicate a serious infection in the skull. The slow onset of significant symptoms is also due to the fact that the dura mater effectively protects the surface of the brain.
It is not infrequently that an epidural abscess is diagnosed only when its complications are suppurative meningitis or brain abscess.
The diagnostic procedure is the same for subdural empyema and epidural abscess. The gold standard is CT of the brain with contrast medium administration and MRI of the brain.
The advantage of MRI scanning is the ability to differentiate these purulent processes from sterile deposits and hemorrhage.
Therapy involves lengthy antibiotic treatment, lasting 3-6 weeks, and surgery or drainage.
Approximately 5-7% of patients die from this serious neuroinfection. The prognosis is particularly poor for patients with impaired consciousness and convulsions. About ⅓ of patients have permanent sequelae after overcoming the infection, which include epilepsy or residual limb paralysis.
How it is treated: Brain abscess
How is a brain abscess treated? Treatment includes antibiotics, surgery
Show moreBrain abscess is treated by
Brain abscess is examined by
Other names
Interesting resources
Related










