- DUBOVÁ, Olga and Michal ZIKÁN. Gynaecology and obstetrics: practical repetition. 2nd edition. 2nd edition: Maxdorf, [2022]. Jessenius Medical Faculty. ISBN 978-80-7345-716-7
- MAREŠOVÁ, Pavlína. Modern procedures in gynaecology and obstetrics. 3rd, revised and supplemented edition. Prague: Institute of Gynaecology and Obstetrics of the CAS, v. v. i.: Medica (Maxdorf). ISBN 978-80-7345-709-9
- urologiepropraxi.cz - Urinary incontinence in pregnancy. Ivan Huvar, CSc.
- Healthline.com - Pregnancy incontinence: why it happens and what to do. Ashley Marcin
- pubmed.ncbi.nlm.nih.gov - Urinary incontinence in pregnancy. Is there a difference between the first and third trimester? National Library of Medicine
Urine leakage in pregnancy and after childbirth: what causes it? 3 exercises you can do at home

Urinary leakage is a common accompanying phenomenon that occurs during pregnancy or after the birth itself. What is the cause of incontinence and what are the options for therapy and prevention?
Article content
Why urine leakage occurs in women, how incontinence can be combated and many other interesting information can be found in the article.
Urinary leakage in pregnancy
A woman undergoes many hormonal changes during pregnancy. The developing baby in the mother's abdomen physiologically expands the walls of the uterus and oppresses the surrounding organs of the cavity with its volume.
In most cases, the growing baby presses on the bladder, which is in close proximity to the uterus.
The bladder has a smaller capacity under the constant pressure of the uterus. The consequence is a sensation to urinate when it is only partially full. In some cases, the kicking of the baby can cause urine leakage due to weakened bladder walls.
Usually, however, it is a few drops of urine.
At the beginning of pregnancy, a woman may experience a frequent sensation to urinate. This phenomenon is also due to increased blood supply to the organs of the small pelvis. To some extent, the angle that the bladder and urethra are clamped changes.
Incontinence in pregnancy, however, predominates in the third trimester of pregnancy due to the significant enlargement of the uterus and the baby.
Approximately 30% of women experience incontinence in pregnancy.
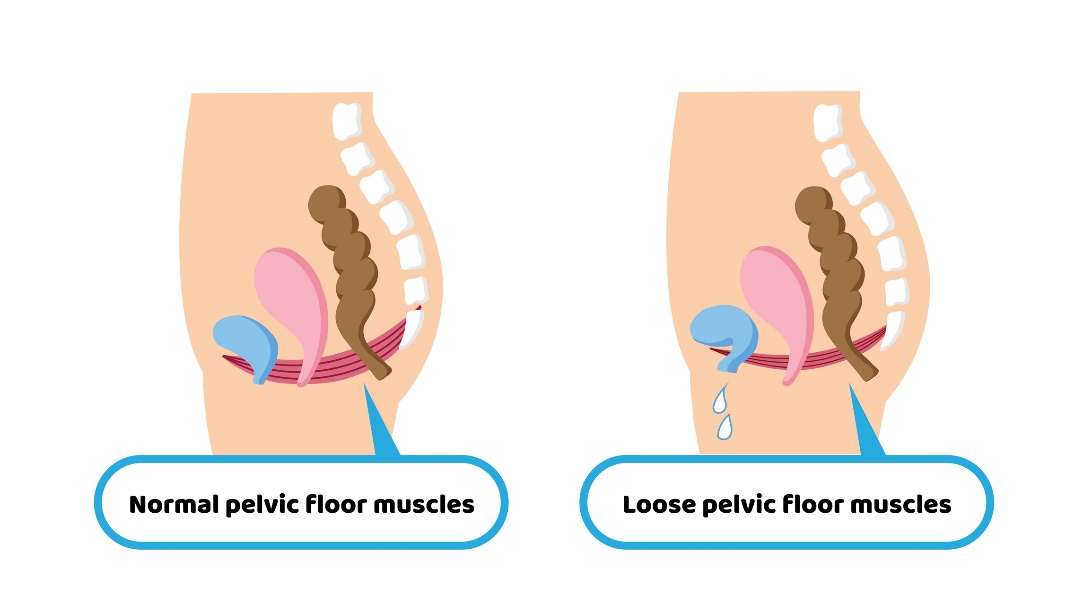
From the constant pressure and growth of the uterus, the pelvic floor muscles subsequently become flaccid and relaxed. The sphincters become slightly flaccid and the pregnant woman experiences incontinence in certain situations.
These are mainly moments such as coughing, sneezing, laughing or jumping.
Most often, it is the leakage of only a few drops of urine. However, in some cases, the incontinence problem may occur with greater intensity. In worse cases, there may be a slight leakage of stool.
Pregnancy, weakened immunity and frequent urination are also associated with the risk of developing an infection or inflammation of the urinary tract. It is therefore advisable to urinate regularly, visit the toilet as soon as possible and follow the principles of intimate hygiene.
If a woman experiences incontinence during pregnancy, a doctor should be consulted to recommend appropriate treatment.
The occurrence of incontinence is individual and depends on a number of factors. However, in a mild form it is common even in healthy women without a certain predisposition.
Not every pregnant woman suffers from incontinence, and not every woman experiences urine leakage at the same time. It can occur at the beginning of pregnancy, at the end of pregnancy or shortly before delivery, sometimes even after the delivery itself.
Factors that increase the incidence of incontinence in pregnancy:
- Higher maternal age
- Multiple births
- Genetic factor
- Weakened pelvic floor
- Muscle imbalance in the pelvic area
- Frequent bladder inflammation
- Urogynecological surgeries
- Exposure to stress
- Diabetes mellitus
- Diseases of the spine and spinal cord
Urinary leakage after childbirth
The subsequent excessive stress on the pelvic organs after pregnancy is the birth itself. A woman's body is physiologically pre-set for the course of labour and subsequent recovery.
With excessive pressure in the second birth canal during the expulsion phase, there is increased pressure on the bladder.
The muscles of the pelvic floor and vaginal cavity must be sufficiently tightened for the delivery to proceed without complications.
In some rare cases, the nerves controlling the bladder may be disrupted during labour, the pelvic floor muscles may be damaged, or labour may be assisted by special forceps. This may subsequently cause postpartum incontinence.
According to the National Institutes of Health, women who give birth naturally vaginally are 50% more likely to develop postpartum incontinence than women who give birth by caesarean section.
However, there are other complications associated with a C-section. You should consult your doctor about the appropriate method of delivery.
After childbirth at the time of the sixth week, the proportions of the abdominal cavity and small pelvis change again. The shrinking uterus gradually reaches its original size.
It is necessary to follow medical instructions, certain lifestyle modification and apply postpartum exercises - rehabilitation to strengthen the pelvic floor and eliminate diastasis of the abdomen.
Factors increasing the incidence of postpartum incontinence:
- Increased maternal age
- Multiple births
- High body weight of the baby
- High preterm birth weight, high birth weight of twins, triplets
- Maintaining pregnancy weight after birth
- Urogynaecological operations
- Physical labour of the mother during pregnancy
- Mental stress
- Diabetes mellitus
- Diseases of the spine and spinal cord
- Weakened pelvic floor
- Muscular imbalance in the pelvic area
Treatment options for urinary incontinence
Exercise during pregnancy should be consulted with a gynecologist due to the woman's individual health, stage of pregnancy, position of the baby, medical history and possible health complications.
Simple, undemanding exercises are chosen for rehabilitation in pregnancy. Their aim is to strengthen, activate and become aware of the pelvic floor, to relieve overloaded muscles of the cervical spine and to familiarise the patient with the ergonomics of movement.
The treatment of incontinence in pregnancy and postpartum depends on its form and severity. If it is a mild leakage of urine due to physiological growth of the uterus or due to a short postpartum period, incontinence aids should be used.
For light leakage, incontinence pads and panties are useful. These are modern, discreet devices that are absorbent and protect against odour and moisture. The wide range available allows the woman to choose the appropriate option according to the size and degree of incontinence (absorption).
The main key to treating postpartum incontinence is special exercises to strengthen the pelvic floor.
Postpartum rehabilitation includes strengthening the pelvic floor muscles, strengthening the abdominal wall and mid-body, teaching proper breathing and correcting movement imbalances in the pelvic area.
The goal of the exercises is to eliminate any prolapse (lowering) of the organs of the excretory system, strengthen the pelvic floor and strengthen the sphincter muscles including the urethra.
Physiotherapists teach women special but simple exercises to activate the pelvic floor. Among those well known among the general public are the Kegel exercises of the American physician, gynaecologist Arnold Kegel.
They focus on the isolated activation of a woman's pelvic floor muscles.
Another option is to train the bladder muscles themselves, which the doctor will explain to the patient in a tailored way. The aim is to gradually increase the time between urination while increasing awareness of the pelvic floor muscles and sphincters.
Vibrating intravaginal devices are also used to strengthen and increase awareness of the pelvic floor. Their aim is to activate the sphincter muscles, increasing sensitivity and awareness of this area.
Their use must be consulted with a gynaecologist, as they are not suitable in pregnancy and in the period shortly after childbirth.
The possibility of surgical treatment is indicated especially in women in whom conservative treatment has failed. These are cases where there is a constant presence of reduction of the organs and pelvic floor, a high rate of incontinence, leakage of stool and other associated health complications.
The choice and type of specific surgery is always individual. The choice of surgery also depends on the recurrent planned pregnancy.
Weakened pelvic floor
Thepelvic floor is a group of muscles forming the cap of the pelvic cavity. Their function is to maintain the correct position, stability and mobility of the organs of the small pelvis (sexual, excretory and digestive systems).
The pelvic floor also plays a large role in the actual function of the organs. For a woman, the pelvic floor is of great importance during pregnancy, childbirth and in the experience of sexuality.
Pelvic Floor Activation Aid.
It is advisable to keep the pelvic floor muscles strong and functional before pregnancy. This reduces the risk of incontinence, postpartum complications and also speeds up recovery time.
Prevention to reduce the risk of incontinence
Prevention to reduce the risk of urine leakage during and after pregnancy starts before pregnancy itself.
It is advisable to have an active, functional pelvic floor, a stable mid-body and plenty of physical activity.
Lifestyle modifications such as limiting smoking, weight control, professional treatment for any medical conditions and, last but not least, elimination of urinary tract infections are advisable.
It is advisable to include exercises targeting the pelvic floor and pelvic region in physical activity to eliminate the subsequent weakening of the sphincter muscles in pregnancy.
3 simple exercises you can do at home to activate the pelvic floor
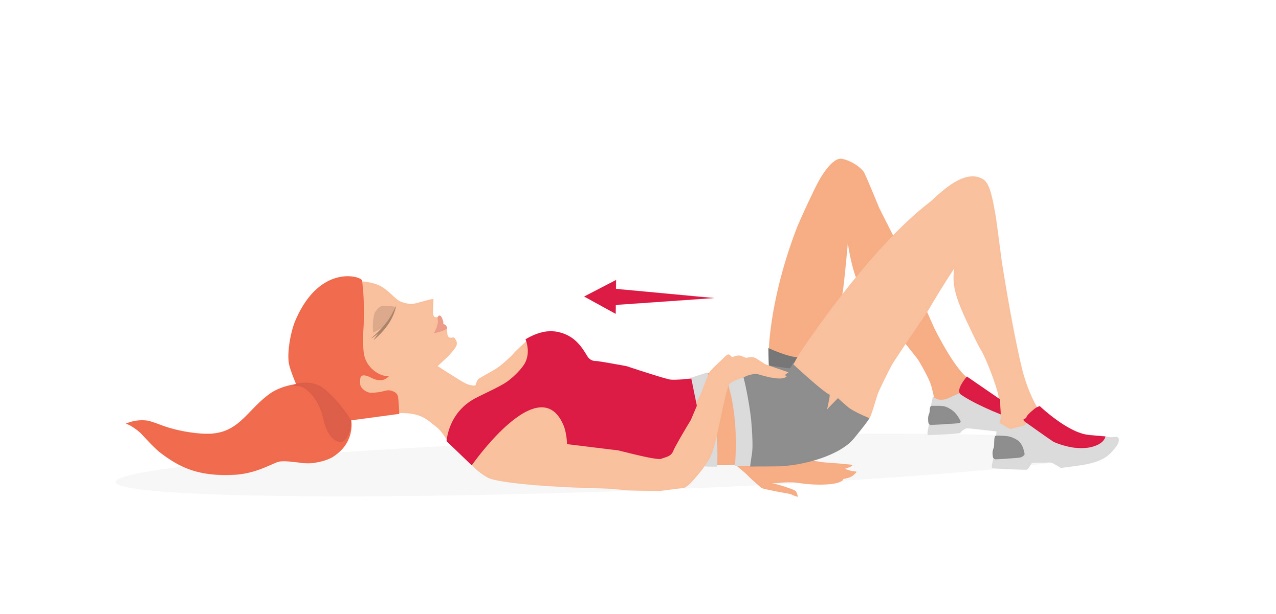
Pelvic floor activation and relaxation
The starting position is lying on your back with the lower legs bent at the knee joints and the feet glued to the mat. The head is in extension of the spine and the shoulders resting loosely on the mat away from the ears.
The purpose of the exercise is isolated contraction of the pelvic floor.
The woman tries to become aware and draw the pelvic floor muscles inward and hold for a moment with smooth breathing into the diaphragm.
She then relaxes the pelvic floor muscles. When activating the pelvic floor, it is recommended to contract each buttock muscle separately and gently tuck the pelvis during the exercise.
The contraction and subsequent relaxation of the muscles can be controlled with the palm of the hand placed under the buttocks.
Be careful not to hold your breath during the exercise and not to feel the pelvic floor area.
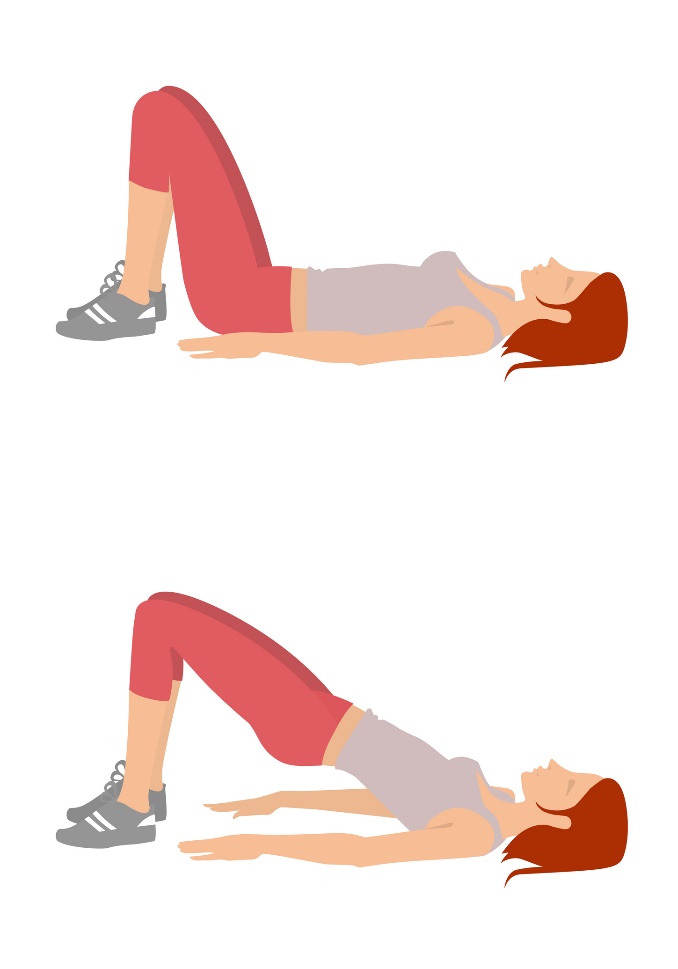
Glute bridge with pelvic floor activation
The basic position is the same as for the previous exercise. Knees bent, shoulder blades resting on the mat and the spine glued to the soft mat. Knee joints are level with the width of the hip joints. Arms are placed loosely by the body, palms down.
The hands are placed loosely on the mat away from the ears. The pelvis is gradually raised and supported towards the ceiling. The shoulder blades remain supported throughout the exercise.
In the upper bridge position, there is an isolated contraction of the pelvic floor muscles and activation of the gluteal muscles.
The woman remains in this activated position for several seconds and breathes freely into the diaphragm.
With an exhalation, the woman again drops to the mat and relaxes the activated muscles.
Beware of holding the breath during the exercise and insufficient activation of the pelvic floor.
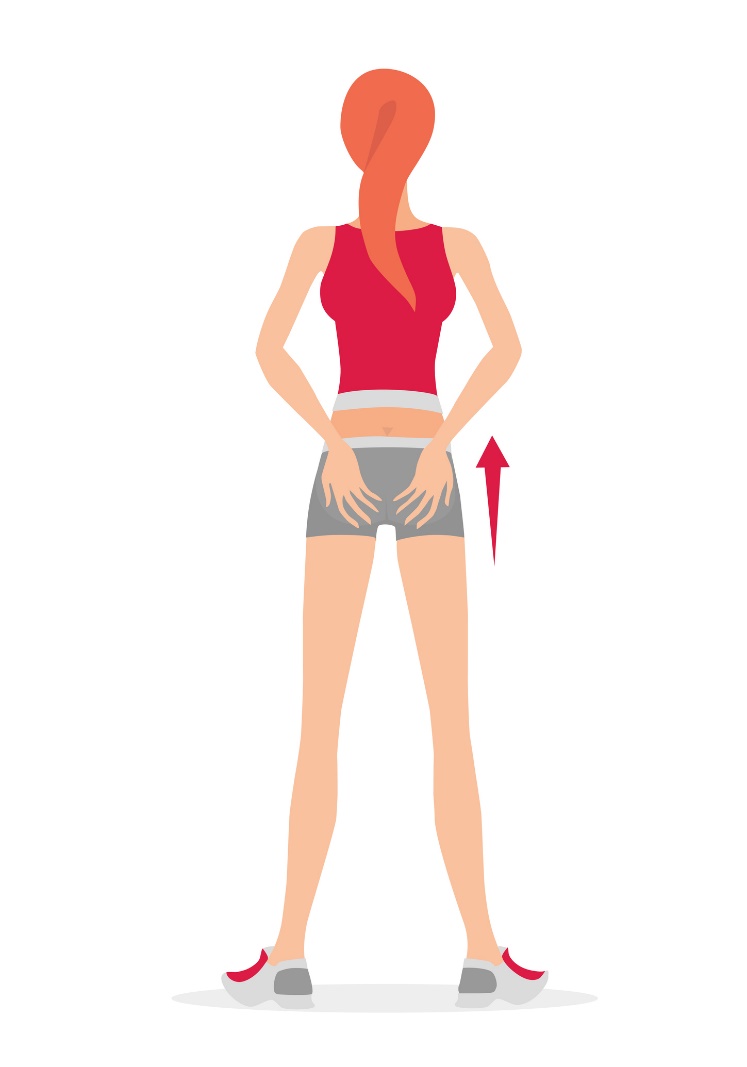
Standing with activation and relaxation of the pelvic floor
The starting position is a slightly staggered standing posture, with the weight of the body resting evenly on both feet. The toes of the feet are pointing slightly apart. The back is in a straight, extended position and the head in an imaginary extension. The shoulders are lowered away from the ears at all times.
The practitioner rests the palms of the hands on the buttocks. The breathing is smooth throughout the exercise. The pelvic floor is activated, contracting the deep inner muscles of the pelvis upwards (inwards).
There is also isolated activation and contraction of the gluteal muscles.
The woman breathes smoothly and tries not to allow the muscles to activate for a few seconds.
Then the activated muscles relax and a pleasant release of tension and relaxation occurs.
Interesting resources










