- pubchem.ncbi.nlm.nih.gov - Phosphorus
- ncbi.nlm.nih.gov - Importance of Dietary Phosphorus for Bone Metabolism and Healthy Aging, Juan Serna, Clemens Bergwitz
- ncbi.nlm.nih.gov - Effects of Excessive Dietary Phosphorus Intake on Bone Health, Colby J. Vorland MS, Elizabeth R. Stremke BS, Ranjani N. Moorthi MD, Kathleen M. Hill Gallant PhD RD
- sciencedirect.com - Acid-Base Problems, Barbara M. Fishman
- sciencedirect.com - Acid-Base, Electrolyte, and Metabolic Abnormalities, Ahmad Bilal Faridi, Lawrence S. Weisberg
- ods.od.nih.gov - Phosphorus
- lpi.oregonstate.edu - Phosphorus, Mona S. Calvo, Ph.D.
- multimedia.efsa.europa.eu - Dietary Reference Values for the EU
- solen.cz - Enteral and parenteral substitution with phosphorus compounds from the pharmacist's point of view, PharmDr. Michal Janů, MUDr. Eva Meisnerová, PharmDr. Jitka Dvořáková, Assoc. PharmDr. Ruta Masteiková, CSc.
- eur-lex.europa.eu - REGULATION (EC) No 1333/2008 OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL on food additives
The role of phosphorus in the body. Is it important for health? Where do you find most of it?

What role does phosphorus play in our bodies? Is it important for maintaining health and why is it needed? What if there is too little or too much?
Article content
- What do we know about phosphorus?
- Occurrence and uses of phosphorus
- What is the biological function of phosphorus?
- The phosphorus pathway - from absorption to excretion
- What are the sources of phosphorus in the diet?
- What is the recommended daily intake of phosphorus?
- What is the consequence of disturbed phosphorus levels?
- Insufficient phosphorus levels
- Excessive amounts of phosphorus
What contains the most phosphorus in case there is not enough of it in the body?
Or...
How to reduce it in case of excess?
What do we know about phosphorus?
Phosphorus is a non-metallic chemical element that is quite abundant in the environment around us. It is an essential mineral for the human body.
We know it by the chemical symbol P. This is derived from the Latin word phosphorus.
The name phosphorus comes from the Greek word phosphoros. It is a combination of the words phos (light) and phoros (light-bearer), referring to phosphorus' ability to glow in the dark.
Phosphorus is an element in Group 15 of the periodic table of chemical elements and is found in Period 3.
It is classified in a group of elements called the pentels, where, in addition to phosphorus, nitrogen, arsenic, antimony, and bismuth are also found.
The discoverer of phosphorus is the German merchant and alchemist Hennig Brand, who first isolated it in 1669.
The discovery itself was preceded by Hennig Brand's efforts to create the legendary Philosopher's Stone.
In his experiments, he worked with clay, first letting it stand for several days and decompose, then boiling it to a paste, heating it to a high temperature and letting the vapours condense.
He thus obtained a white waxy substance that glowed in the dark - phosphorus.
Phosphorus exists in several forms. We speak of its allotropic modifications, which differ greatly in their properties.
The two most common forms are white phosphorus and red phosphorus. But in addition to these, we also know yellow, black or violet phosphorus.
White phosphorus is a white, soft, waxy solid. In its pure form it is transparent. It is insoluble in water. Of all the forms of phosphorus, white phosphorus is the least stable, the most reactive, the least dense and the most toxic.
It has the ability to glow in the dark and can spontaneously ignite on contact with air. It must therefore always be immersed in water.
The light emission of phosphorus is due to its slow oxidation in air. This process is called chemiluminescence.
Because of the tendency of phosphorus left in the air to ignite spontaneously, it is sometimes referred to as the devil's element.
Yellow phosphorus represents the so-called intermediate between white and red phosphorus. It is white phosphorus that contains small amounts of red phosphorus.
Red phosphorus is an amorphous solid. It is formed from white phosphorus by a heating process or by exposure to sunlight. It is less toxic, less reactive and more stable.
Black phosphorus is the most stable and least reactive form of phosphorus. It is also obtained from white phosphorus by heating, but in the presence of mercury.
A tabular summary of basic chemical and physical information about phosphorus
| Name | Phosphorus |
| Latin name | Phosphorus |
| Chemical name | P |
| Classification of elements | Pentels/pnictides |
| Grouping | Solid (at standard pressure and temperature) |
| Proton number | 15 |
| Atomic mass | 30,973 |
| Oxidation number | -3, +3, +5 |
Occurrence and uses of phosphorus
Phosphorus is the twelfth most abundant element in the Earth's crust. It is also found in space (e.g. as part of meteorites), in soil, rocks or in plants and animals.
Due to its reactive nature, it does not occur in nature in free form. It is largely found in minerals, in the form of phosphate ions or phosphate salts.
The best known minerals containing phosphorus are apatite (these minerals are also the most important natural sources of phosphorus), wavellite or vivianite.
Organic sources of phosphorus include urine, bone ash or guano (accumulated excrement from seabirds or bats).
Phosphorus and its compounds are used in many areas and industries today. For example:
- Preparation and production of various phosphorus compounds
- Production of fertilizers and pesticides
- Manufacture of matches, porcelain, fireworks or smoke bombs
- As a component of cleaning agents and anti-corrosive agents
- As a water softener
- Use in beverages and baking powders
- As a radiolabel in biochemical tests

What is the biological function of phosphorus?
Phosphorus is an essential nutrient for human health and has many physiological functions in the body.
The human body contains on average 0.7 kg of phosphorus.
The vast majority of phosphorus (up to 85%) is part of the hydroxyapatite molecule Ca10(PO4)6(OH)2, which is the mineral that forms the most important component of the hard tissues of bones and teeth.
The remaining phosphorus is found in soft tissue cells (approximately 15 %) and in extracellular fluid, mainly blood (approximately 1 %).
In terms of chemical structure, phosphorus is most commonly found in the body as an inorganic ion, HPO42- or H2PO4-. These are salts of phosphoric acid, also called phosphates.
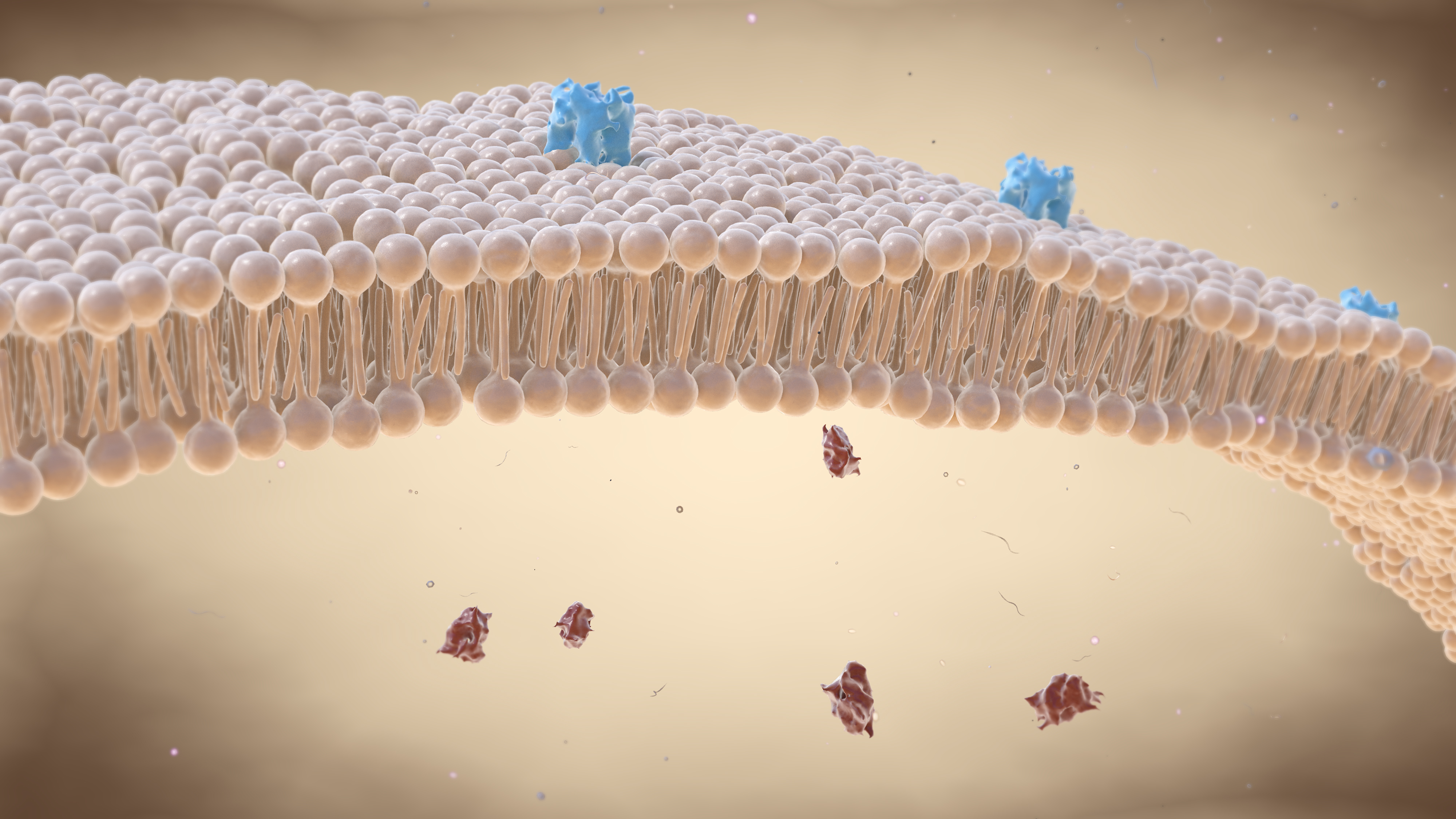
However, it can also be bound in compounds such as membrane phospholipids, DNA and RNA nucleic acids, ATP, creatine phosphate or various other organic molecules.
The basic biological functions of phosphorus in the human body include:
- It is an important component of bones and teeth. It is involved in their mineralization, thus ensuring their strength and hardness.
- It is a component of the ATP molecule, adenosine triphosphate, a chemical compound that is the primary reservoir and source of energy for the body's cells.
- It is a component of the nucleic acids DNA and RNA. In them is stored the genetic information of an individual.
- As part of the phospholipid molecule, it is an essential building block of cell membranes and ensures their structural integrity.
- As an extracellular ion, it is involved in maintaining normal pH and acid-base balance.
- It is a component of carbohydrates and is involved in the metabolic conversion of proteins and fats.
- It activates various enzymes.
The phosphorus pathway - from absorption to excretion
Absorption
The primary source of phosphorus for the body is food. Both inorganic and organic forms of phosphorus are absorbed from food in the digestive tract. The inorganic form predominates.
The availability of phosphorus to the body depends on the nature of the food. The lowest availability is from plant protein foods, followed by animal protein foods, and the highest availability is from food additives containing inorganic phosphorus.
Phosphorus is absorbed in the small intestine and, to a lesser extent, in the large intestine by two routes - diffusion without energy (up to 70% of the fraction) or via sodium-dependent transporters.
The rate of intestinal absorption of phosphorus is relatively high, at 50-70% of the total phosphorus present in the diet.
Cervical absorption of phosphorus is significantly higher in infancy (up to 90 %). The rate of absorption slowly decreases with age.
The remaining phosphorus that is not absorbed in the digestive tract is excreted in the faeces.
In total, about 13 mg phosphorus/kg body weight per day is absorbed from food into the blood via the digestive tract. This amount is subsequently utilised by the tissues.
A smaller amount, about 3 mg phosphorus/kg body weight per day, is excreted from the body in bile, pancreatic secretions and intestinal secretions.
Phosphorus absorption can be reduced by various disorders and diseases such as kidney failure, kidney stone formation, absorption disorders in the small intestine, thyroid disease or osteomalacia (bone disease).
Distribution and regulation of phosphorus levels
Absorbed phosphorus circulates in the blood and reaches the sites of utilization - mainly bone, skeletal muscle, soft tissue and kidney.
Phosphorus is transported to the tissues as an inorganic ion. The extent of this transport depends on the concentration of phosphorus in the blood, the rate of blood circulation and the activity of cellular transporters.
Bones are the largest reservoir of phosphorus. From them, phosphorus can be released back into the blood when needed.
Normal blood phosphorus levels in an adult range from 0.7 to 1.45 mmol/l.
Upward or downward deviations from this level are the cause of disorders in the body. For this reason, the total amount of phosphorus in the body must be regulated.
Tissues and organs, but also biologically active substances - hormones - are involved in maintaining phosphorus homeostasis.
Of the organs, these are mainly the kidneys, parathyroid glands, corpuscles and bones. The hormones are parathyroid hormone, fibroblast growth factor-23 and vitamin D.
These regulate phosphorus levels by affecting its absorption in the digestive tract, excretion by the kidneys and release from body stores (bone or cellular).
The process of maintaining homeostasis is as follows. When there is a slight drop in blood phosphorus levels, this change is detected by the parathyroid glands. The parathyroid glands respond by producing parathyroid hormone.
This stimulates the release of phosphorus from the bones into the blood and also the production of the active form of vitamin D. Vitamin D then increases the absorption of phosphorus in the digestive tract.
At the same time, the production of fibroblast growth factor-23 (produced in the bones) is reduced, thus reducing the excretion of phosphorus by the kidneys.
Conversely, an increase in blood phosphorus levels will increase the production of fibroblast growth factor-23. This will stimulate renal excretion of phosphorus. At the same time, however, vitamin D production will be reduced and thus phosphorus absorption in the gastrointestinal tract will be reduced.
The level of phosphorus in the blood or other body fluids is determined by its reaction with ammonium molybdate to form ammonium phosphomolybdate.
Excretion
The kidneys are responsible for excreting phosphorus from the body. This means that the primary route of phosphorus excretion is urine.
More than 5 000 mg of inorganic phosphorus ions are filtered through the kidneys every day. More than 80% of these are returned to the blood.
The kidneys are also the main organ regulating the concentration of phosphorus in the blood.
Small amounts of phosphorus and its compounds that are not absorbed in the digestive tract are excreted in the faeces.
What are the sources of phosphorus in the diet?
Phosphorus enters the body mainly through food, and to a lesser extent through supplements or medicines.
Phosphorus is present in foods either as a natural part of the food or is deliberately added during production and processing in the form of inorganic phosphates.
Foods naturally high in phosphorus are animal meat, fish, dairy products, eggs, cereals, nuts, seeds, legumes and vegetables. The intake of these foods can cover most of the daily phosphorus requirement.
Some, and sometimes not insignificant, amounts of phosphorus also enter the body through foods or beverages to which phosphates are intentionally added.
The most well-known examples are flavoured soft drinks, meat products, fish, milk and dairy products, vegetable oils, flour, baked goods, ice cream, processed vegetables and nuts, sweets, diet foods, frozen foods, mineral waters, wine and spirits, etc.
Phosphates act as stabilizers, emulsifiers, raising and moistening agents and thickeners.
Tabular list of permitted additives containing phosphorus in foods
| E number of the additive | Name of the additive |
| E338 | Phosphoric acid |
| E339 | Sodium phosphates |
| E340 | Potassium phosphates |
| E341 | Calcium phosphates |
| E343 | Magnesium phosphates |
| E450 | Diphosphates |
| E451 | Triphosphates |
| E452 | Polyphosphates |
Certain foods, food ingredients and even medicines can significantly reduce the availability of phosphorus to the body. This occurs, for example, by inhibiting its absorption, affecting the pH in the digestive tract, etc.
Phytic acid or phytate is the main source of phosphorus in seeds or plants. Phytate binds with other compounds in the digestive tract to form salts that are indigestible by the body.
In addition, the human body does not have the enzyme phytase to break down the phosphorus bond in the phytate molecule.
Also, the high intake of calcium in the diet causes it to bind to some of the phosphorus compounds. This reduces its absorption.
Of the drugs, some antacids (drugs used to reduce the acidity of gastric juice) such as sucralfate, magnesium hydroxides or aluminium hydroxides bind to phosphorus in the diet. They form unabsorbable salts with it.

What is the recommended daily intake of phosphorus?
Recommendations for the average daily intake of phosphorus have not been established due to the lack of data.
However, the European Food Safety Authority publishes values for adequate phosphorus intake. Adequate intake is an average value based on observation. It is assumed to correspond to the needs of the population.
Table of adequate daily intakes of phosphorus by age
| Age group | Adequate phosphorus intake |
| Infants (aged 7-11 months) | 160 mg/day |
| Children aged 1-3 years | 250 mg/day |
| Children aged 4-10 years | 440 mg/day |
| Adolescents aged 11-17 years | 640 mg/day |
| Adults (age = 18 years) | 550 mg/day |
| Pregnant women (age = 18 years) | 550 mg/day |
| Breastfeeding women (age = 18 years) | 550 mg/day |
The current trend in nutrition is that these phosphorus levels are exceeded several times over.
What is the consequence of disturbed phosphorus levels?
Phosphorus levels are and must be strictly regulated in the body. However, under certain circumstances, deviations from normal blood phosphate levels do occur.
Significant and prolonged deviations are considered a non-physiological condition. They can be the cause of various health complications.
Two situations can occur: the occurrence of excessive amounts of phosphate in the blood (hyperphosphatemia) or, conversely, a lack of phosphate (hypophosphatemia).
Insufficient phosphorus levels
The occurrence of phosphorus deficiency in the body is a relatively rare condition. There can be several causes of hypophosphatemia, but it is almost never caused by insufficient dietary phosphorus intake.
It is primarily due to the diet containing sufficient natural or deliberately added phosphorus. It may also be due to a well-functioning regulation of homeostasis, where a reduction in dietary phosphorus intake as a compensatory mechanism reduces its excretion by the kidneys.
Hypophosphatemia is said to occur when blood phosphorus levels fall below 0.7 mmol/l.
A mild decrease in phosphorus levels does not have visible or noticeable symptoms in humans. Symptoms only appear when there is a significant decrease, i.e. below 0.15 mmol/l.
The most common general symptoms of hypophosphatemia include weakness, malaise, impaired sensitivity of the limbs, tremor, loss of appetite.
Muscle symptoms include incoordination, flaccidity to complete muscle paralysis and rhabdomyolysis (a disorder characterised by the breakdown of skeletal muscle fibres).
There is also bone pain, bone mineralisation disorders leading to rickets in children and osteomalacia in adults (bone disease characterised by softening and deformation of the bones), anaemia, white blood cell and platelet disorders, increased susceptibility to infection, respiratory problems or oxygen deficiency and heart disease.
Severe forms of phosphorus deficiency can be life-threatening.
The main causes of hypophosphatemia include:
- Insufficient dietary phosphorus intake - this can lead to starvation conditions
- Disorders of phosphorus absorption - malabsorption, Crohn's disease, inflammatory bowel disease
- Insufficient intake of vitamin D, which reduces phosphorus absorption in the blood
- Increased renal excretion of phosphorus
- Diseases of the parathyroid glands
- Hormonal changes
- Heavy metal poisoning
- Decreased potassium and magnesium in the blood, high blood glucose levels
- Excessive alcohol consumption
- Certain medications (e.g. antacids, diuretics, steroid hormones, parathyroid hormone)
The use of hormone replacement therapy in postmenopausal women is associated with increased excretion of phosphorus by the kidneys, thus lowering phosphorus levels in the body.
There are also several population groups that are considered to be at risk in terms of developing reduced or insufficient levels of phosphorus in the body. For example:
- Premature babies (who have low phosphorus stores in their bones)
- People with inborn errors of phosphorus metabolism (disorder of hormones responsible for regulating phosphorus homeostasis, disorder of phosphorus transporters)
- People with severe malnutrition (low birth or body weight, anorexia, alcoholism, chewing and swallowing problems, cancer, cirrhosis, etc.)
- People eating a diet high in calories and low in phosphorus
How to treat hypophosphatemia?
Phosphorus deficiency is primarily treated by increasing dietary phosphorus intake or taking appropriate medications and supplements containing phosphorus.
The specific method of phosphorus supplementation always depends on the severity of the deficiency and the health of the patient.
For mild to moderate phosphorus deficiency, the intake of foods high in phosphorus (skimmed milk is suitable) or the use of medicines and supplements (e.g. for patients with milk intolerance) is sufficient.
Pharmaceutical preparations containing phosphorus are available in monocomponent form (usually prepared separately in a pharmacy) or in combination form (in the form of multivitamin or mineral supplements).
Phosphorus is most commonly found in the form of sodium, potassium or calcium salts of phosphoric acid.
Multivitamin or mineral supplements usually contain small amounts of phosphorus and are therefore not primarily used to treat phosphorus deficiency.
Administration of phosphorus-containing supplements is often associated with the occurrence of diarrhoea.
In severe phosphorus deficiency or in patients who are unable to take phosphorus by mouth, parenteral (intravenous) administration is resorted to.
Parenteral administration of phosphorus must be monitored because of the possible formation of calcium phosphate crystals and the risk of calcium deficiency. The use of potassium phosphate or, better still, organic salts of phosphorus is preferable and eliminates the problem of crystal formation.
Excessive amounts of phosphorus
Hyperphosphatemia is a condition where the blood phosphorus level rises above 1.6 mmol/l.
The occurrence of high levels of phosphorus in the body is relatively rare in healthy individuals. When excessive amounts of phosphorus are ingested in the diet, regulatory mechanisms excrete the excessive amounts through the kidneys.
The presence of high phosphorus levels is associated with impaired phosphorus excretion. This means that hyperphosphatemia is most often associated with impaired kidney function or kidney disease.
The main causes of hyperphosphatemia include:
- Increased phosphorus intake (e.g. intravenously).
- Excessive intake of vitamin D, which increases phosphorus absorption in the intestines
- Rapid release of phosphorus from cells and tissues into the blood
- Impaired renal excretion of phosphorus (in renal failure or chronic kidney disease)
- Inflammation of the pancreas
- Disease of the parathyroid glands
- Rhabdomyolysis, tumor breakdown syndrome (metabolic disruption caused by the sudden breakdown of tumor cells during tumor treatment)
Among the most important consequences of elevated blood phosphorus levels is an increase in parathyroid function and the associated increase in parathyroid hormone production.
In order to maintain homeostasis, the body tries to reduce excessive phosphorus levels in the blood by excreting phosphorus through the kidneys. However, when kidney function is impaired, this effort is futile. It leads to the production of unnecessarily high amounts of parathyroid hormone.
A high level of phosphorus in the blood also leads to its reaction with calcium to form crystals of calcium phosphate, which are deposited in the soft tissues of the body.
This causes calcification of soft tissues, including subcutaneous and nervous tissue or blood vessel tissue. The consequence is the development of vascular and heart disease.
Hyperphosphatemia also causes the development of low blood calcium levels.
Excess phosphorus itself usually has no symptoms. Symptoms appear when calcium levels are significantly reduced due to elevated phosphorus levels.
We speak of hypocalcemia. Thus, symptoms of hypocalcemia may also be related to hyperphosphatemia.
Excess phosphorus also causes a reduction in magnesium levels, further impairs kidney function and can cause kidney failure.
How to treat hyperphosphatemia?
Several procedures are used in the treatment of excess phosphorus in the body.
Its intake and absorption can be regulated by a reduction diet with reduced dietary phosphorus intake or by the use of phosphorus-binding substances in the environment of the digestive tract that form unabsorbable complexes (e.g., aluminum hydroxide, aluminum carbonate).
Renal excretion of phosphorus into the urine may also be increased by the use of diuretics (only if the patient has normally functioning kidneys).
Patients with hyperphosphatemia who also have kidney damage usually undergo dialysis.
Interesting resources
Related










