- solen.cz - superficial candidiasis and treatment options
- uvzsr.sk - fungi
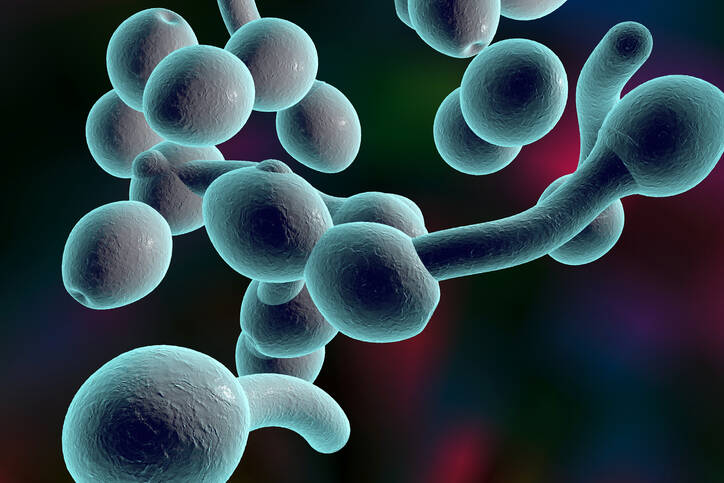
- wikipedia.cz - candida albicans
- solen.sk - mycotic skin diseases
- solen.sk - superficial mycoses
Parasitic fungus, candidiasis: can skin fungus harm the organs?
The ubiquitous fungus afflicts adults and children alike, from the newborn period onwards. Fungal diseases can be both trivial and serious. The most common ones include foot fungus or vaginal mycosis. Rarely, organ involvement can occur in weakened individuals, when an initially harmless fungus becomes a dangerous parasite. The manifestations of mycotic infections are so varied that they are not always easy to recognise. They are often confused with other infections.
Article content
Fungal diseases affect both adults and children. The disease can manifest itself on the skin and mucous membranes, nails and, exceptionally, on internal organs. The most diverse manifestations occur under certain conditions that create a favourable environment for these fungi to multiply.
Candidiasis

Candidiasis is a relatively common fungal disease caused by various fungal agents.
Mycoses have been known since 1837 and there are currently over 200 known species. However, only 12 of them cause the disease.
Interesting:
The mysterious deaths of actress Brittany Murphy in December 2009 and her husband Simon Monjack just a few months later were covered by the media. Investigators initially refused to admit that a fungus found in their home was responsible for the popular couple's early demise. However, it was the fungus that caused the respiratory problems they eventually succumbed to.
Mycoses are the most commonly encountered fungal diseases caused by the yeast Candida albicans, despite the fact that the number of non-albicans candida diseases has been increasing over the last decade. The filamentous fungus Aspergillus fumigatus is also a common cause of mycoses.
Non albicans candidiasis includes fungal diseases caused, for example, by yeast:
- Candida Parapsilosis
- Candida Tropicalis
- Candida Glabrata
- Candida Krusei
- Candida Species
- Candida Hamata
- Candida Guilliermondii
- Candida Lusitaniae
- others
Filamentous fungi causing fungal diseases include
- Fusarium Species
- Zygomycetes
- Scedosporium species
- others
Important: Fungal diseases, affecting mainly the skin and mucous membranes, can alarm us with a breakdown of the body's immunity due to various disease causes (AIDS, diabetes or other serious diseases). Therefore, in addition to self-treatment of mycosis with over-the-counter drugs, it is necessary to search for the cause of the reduced immunity and the subsequent fungal infection.
The human body and fungi
Fungi have always been part of the body's natural microflora (saprophyte). They live in symbiosis with other microorganisms found on the surface of the human body, mucous membranes or internal organs.
The colonisation of the human body by fungi occurs already in newborn babies, at the time of birth. Most often they colonise the oral and intestinal mucosa. Normally they do not cause any health problems and people are not aware of the presence of fungi.
The problem arises when they overgrow under certain specific circumstances, when disease manifestations occur. This happens mainly when immunity is reduced due to other disease causes, especially opportunistic diseases (cancer, AIDS).
Obese people or pregnant women are also a risk group. The use of certain drugs also provides suitable conditions for their multiplication.
Basic classification of mycoses:
- superficial mycoses - fungi on the skin, mucous membranes and nails, for example.
- systemic (organ) mycoses - lung mycoses, fungal diseases of the urinary tract
Fungi in the outdoor environment
Microscopic fungi are almost everywhere around us. In addition to colonizing the surface of skin, mucous membranes, and human organs, they also infect animals and plants. They occur in water (standing surface water, reservoirs of water), in soil, and are dispersed in the air.
They are also found on inanimate objects (walls, bathrooms, toilets, showers, waste, food, dirty hands).
Interesting: mould is all around us. Almost everyone has seen it. A good example is long-forgotten bread, on which a greenish-whitish film forms. This is visible even to the naked eye.
A beneficial mould discovered through the mess
The positive effects of mould were discovered by the famous physician Alexander Fleming, not because of his knowledge, but because of the mess he left in his laboratory in 1928.
After returning from a holiday, he noticed that there was mould on the unwashed culture plates. The bacteria that had been cultured were no longer there.
So he discovered that the mould produced an antimicrobial substance that killed the bacteria. He then isolated it. The resulting product was the antibiotic penicillin (PNC), which is still considered the most effective today.
Fungal diseases of newborns and infants - soor
Fungal disease of newborns and infants is very often encountered. Manifestations of candidiasis occur most often in newborns around the second week of life. It is referred to as soor.
In infants and toddlers, we see fungal disease of the skin and folds in the area where the airless diaper presses against the skin. These areas are ideal environments (warm and moist) for yeast to overgrow.
Prevention is buying only good quality diapers, storing them properly in a dry environment, and changing them regularly to keep baby's bottom dry.
It is less common in the armpits or neck area of chubby babies.
Soor and infant candidiasis - clinical picture
Soor (also known as frog or powdery mildew) typically appears on the mucous membrane of the oral cavity, mainly on the palate, tongue and cheek. The disease manifests itself in the form of white so-called milk spots that cannot be wiped off. They bleed and are painful if removed mechanically.
Fungal disease of infants and toddlers in the skin folds may initially resemble ordinary diaper rash. The skin is red and softened in colour and has small cracks. The underlying skin is milky in colour with blisters.

Fungal diseases of the skin and mucous membranes
Infections of the skin and mucous membranes (mucocutaneous mycoses) tend to be separate or occur together. Mycotic deposits cause superficial but also deeper damage to the skin covering. Very often they occur in weakened (immunodeficient) patients.
Inadequate hygiene, excessive sweating, tight, airless clothing or disturbance of the skin's natural acidity (pH) are also common causes.
Symptoms of fungal diseases of the mucous membranes and skin
The manifestations of mycotic disease are identical to those in newborns (soor). Blistering with a white base appears on the skin. When the blisters burst, a circumscribed deposit is formed which is shiny and red. Cracks form in the deposit and the surface layer of the skin also peels off.
The mucous membranes manifest whitish lesions. The patient feels dryness and scratching in the affected area. Later, itching and even soreness.
Painful swallowing, for example, when the mucous membrane of the oral cavity is infected, causes lack of appetite and difficulty in eating.

Fungal nail disease - onychomycosis
Fungal nail disease is more common on the feet (up to seven times more common than on the toes), but can also occur on the hands. Fungal nails are also found on the extremities, where they mainly affect the fingers and are not uncommon.
Nail mycosis accounts for more than 50% of nail diseases that cause nail change and destruction.
Onychomycosis is spread by direct contact or can even be contracted in places where it is damp and warm (communal showers, swimming pools, tropical areas). It can also develop from wearing tight and unventilated shoes and improper hygiene.
What does nail mycosis look like?
The disease is most often found in people with increased sweating of the feet. At first, there is an initial itching, the skin in the affected area is red and macerated (softened). Later, it may crack, with tiny tears in the skin (ragades) being visible.
The fungus spreads to the nail bed. Its surface becomes yellow to brown in colour (as if dirty). The nail is thickened, brittle and transverse grooves are present. Eventually, hyperkeratosis, deformation, loss of cuticle and disintegration occur.

Fungal disease of the vagina
Inflammatory disease of the vagina caused by fungi is one of the most common gynecological problems. Manifestations of vaginal mycosis are a frequent reason to visit a gynecological outpatient clinic.
There are many factors that trigger this disease (medication, stress, pregnancy, obesity, diabetes, AIDS). However, the fact remains that the vagina is an ideal predilection site for mycoses and other diseases (e.g. bacterial diseases) in terms of temperature and humidity.
How does vaginal mycosis manifest itself?
The most unpleasant symptom, which bothers the patient day and night, is an uncomfortable itching of the vagina and the external genital area. There is a thick discharge of watery consistency or, more often, a thick, white, curd-like discharge with a sour smell. Locally, redness and swelling are present. There are whitish plaques in the vagina, similar to those seen in newborns with soor.

Fungal diseases affecting internal organs
Fungal diseases affecting the internal organs are also called invasive systemic mycoses. The invasion of the system by fungi occurs due to a decrease in the general or local immunity of the person. The number of such patients is constantly increasing, due to the increased number of immunodeficient people.
The groups of people at risk include:
- newborns at risk (low birth weight)
- elderly patients (over 70 years of age)
- patients with AIDS (acute immunodeficiency syndrome)
- patients receiving immunosuppressive therapy (immunosuppressive drugs - organ transplants, haematopoietic cell transplants)
- patients receiving long-term treatment with antibiotics
- patients on long-term steroids
- patients with congenital but also acquired immunodeficiency
- patients with cancer and subsequent aggressive treatment (chemotherapy, corticotherapy)
- patients suffering from leukaemia
- patients with blood malignancies
- patients with severe diabetes and ketoacidosis and renal failure
- patients with cystic fibrosis
- patients with cytomegalovirus infection
- patients after repeated major surgical procedures
- patients with extensive burns
- patients after severe multiple organ system injuries
- patients with a history of invasive mycosis
Organs most commonly affected by yeast:
- bloodstream infected with fungi
- respiratory system infected by fungi
- urinary system infected with fungi
- chronic disseminated form of the disease
Treatment of fungal diseases
The treatment of fungal diseases enjoys a success rate of up to 90%. This is due to the wide range of antifungal drugs available on the market today. Hygiene must be an integral part of the treatment, but also lifestyle modification and, in some cases, treatment of the underlying disease.
Treatment options for mould:
- local (topical) therapy - the drug is applied locally to the affected area in the form of a solution, cream or ointment.
- general (systemic) therapy - used if local therapy is not successful or if there are repeated and frequent recurrences of the disease
Antifungal agents used in the treatment of moulds
The treatment of mycoses depends on several factors. The cause of the lowered immunity and the reason why the fungus has appeared is paramount. Equally important is the age and current condition of the patient. Also, the doctor (dermatologist) must be experienced to make the correct diagnosis.
Antifungal drugs are usually used in a broad-spectrum manner. They work by stopping the mycosis cells from dividing, thus stopping their growth and further multiplication. They act on actively growing fungi, not on spores (so-called dormant cells). The duration of treatment should be followed according to the doctor's advice - usually 2 to 3 weeks.
Imidazole preparations are the first choice for the treatment of mycoses. This group includes, for example, ketoconazole. Triazole derivatives such as fluconazole, itraconazole and posaconazole or echinocandins such as caspofungin and micafungin are also suitable.
Probiotiká v boji proti plesniam
Interesting resources
Related










