- ncbi.nlm.nih.gov - The Global Epidemic of the Metabolic Syndrome, Mohammad G. Saklayen
- my.clevelandclinic.org - Metabolic Syndrome
- nhlbi.nih.gov - Metabolic Syndrome
- mayoclinic.org - Metabolic Syndrome
- solen.cz - Metabolic syndrome, its diagnosis and treatment options, MUDr. Petr Sucharda, CSc.
- solen.sk - Metabolic syndrome, cardiovascular and metabolic risks, prof. MUDr. Peter Galajda, CSc.
- internimedicina.cz - Metabolic syndrome, prediction and prevention, MUDr. Šárka Svobodová, Ph.D., prof. MUDr. Ondřej Topolčan, CSc.
- solen.sk - Metabolic syndrome in children and pitfalls of its diagnosis, MUDr. Eva Vitáriušová, PhD., doc. MUDr. Ľudmila Košt'álová, CSc., mim. prof., MUDr. Zuzana Pribilincová, CSc., MUDr. Anna Hlavatá, PhD., MUDr. Katarína Babinská, Jr., prof. MUDr. László Kovács, DrSc., MPH
What is metabolic syndrome and what are its most common complications?

Metabolic syndrome is a group of disorders in the body that are a risk factor for cardiovascular disease. These disorders always occur together. It poses a health threat.
Most common symptoms
- Headache
- Joint Pain
- Leg Pain
- Spirituality
- Sugar in urine
- Gaining weight
- Overweight
- Swelling of the limbs
- High blood pressure
- Increased appetite
- Increased blood sugar levels
Characteristics
We are talking about five disorders:
elevated blood pressure
high blood sugar
excessive body fat around the waist
elevated cholesterol and triacylglycerol levels in the blood
These pathological disorders always occur together. If only one of these disorders affects you, it is not metabolic syndrome. Metabolic syndrome is a major health threat today, especially because of the rapid and dramatically increasing number of people with this syndrome worldwide.
Metabolic syndrome is not a disease in itself. It is a set of multiple symptoms that occur simultaneously in the body, not randomly.
The adjective "metabolic" refers to its association with biochemical processes naturally occurring in the human body.
We speak of a metabolic syndrome when any of the following five non-physiological conditions coexist in the body:
- High levels of sugars (specifically glucose) in the blood
- Low levels of HDL cholesterol in the blood
- High levels of triacylglycerols (fats) in the blood
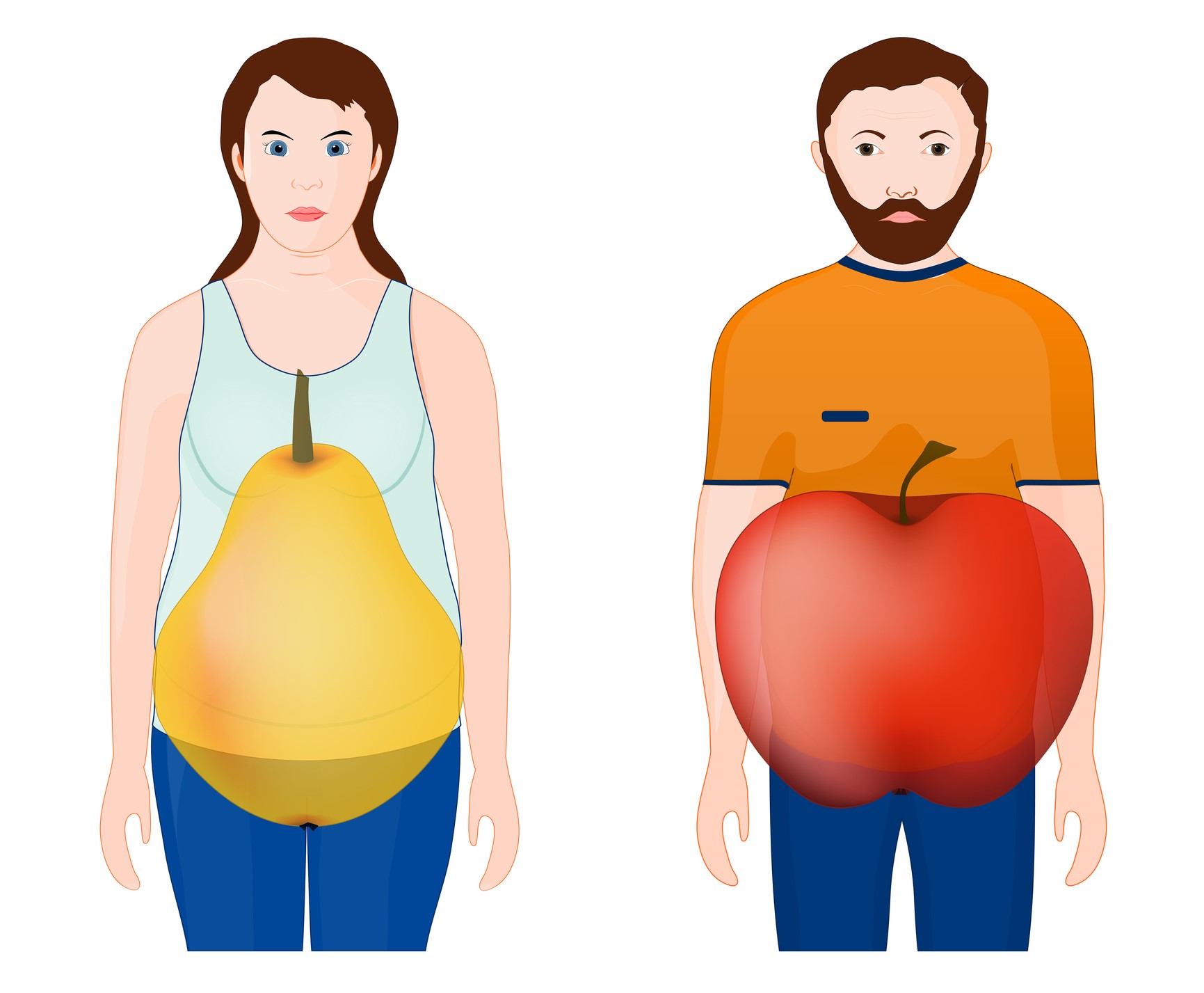
- Accumulation of body fat in the waist area, causing the typical "apple" or "pear" body shape
- High blood pressure
The occurrence of these disorders is the result of other factors. Most often these are lifestyle-related factors, but also genetics or a disorder called insulin resistance.
They also pose a significant risk for the development of heart disease, atherosclerosis, type 2 diabetes, stroke, as well as other serious health problems.
If you experience three or more of these disorders at the same time, there is a high likelihood that metabolic syndrome is affecting you.
Simple math applies here too.
The more of these disorders you develop, the higher your risk.
Complications of metabolic syndrome
A developed metabolic syndrome in the body that is not adequately compensated for poses a danger, especially in terms of possible progression to more serious and life-threatening conditions.
The most common consequences mentioned in relation to metabolic syndrome are heart disease and type 2 diabetes.
Read also:
What health complications does diabetes cause?
Hyperglycaemia: How does excess blood sugar manifest itself and what is the treatment?
Heart disease resulting from metabolic syndrome can lead to heart attack.
As a result, fatty particles are deposited in the blood vessel walls and atherosclerotic plaques form.
The blood vessels are narrowed or even blocked, and the heart's blood and oxygen supply is significantly reduced, most commonly manifested by chest pain.
Type 2 diabetes arises when the body's cells are unable to take up sugar (glucose) from the blood and are resistant to insulin. Alternatively, it can arise when not enough insulin is produced in the body.
The unconsumed glucose builds up in the blood and causes a gradual breakdown of the body.
Another health consequence of this syndrome is kidney damage, particularly the kidneys' reduced ability to excrete salts from the body.
We can also mention the increased risk of blood clots or excessive fat deposition in the liver, so-called fatty liver, which is associated with the occurrence of liver inflammation.
A look at the history of...
The co-occurring conditions of diabetes, obesity and high blood pressure were known in earlier times. Even then, people noticed the link between them.
For example, the occurrence of diabetes resulting from an underlying obesity had already been described in antiquity.
The foundations of the current definition of metabolic syndrome were laid by the American internist and endocrinologist Gerald M. Reaven in 1988. He was mainly concerned with insulin resistance. In conjunction with this, he demonstrated that the relationship between insulin, glucose, triacylglycerols, HDL cholesterol and elevated blood pressure is not coincidental.
At the time, the syndrome was called syndrome X.
Until 1999, the metabolic syndrome lacked a uniform and universally accepted definition, even though it had been the subject of research much earlier.
The World Health Organization (WHO) finally came up with one that year.
The WHO definition of metabolic syndrome is as follows.
It is a pathological condition characterised by abdominal obesity, insulin resistance, high blood pressure and high blood fat content.
In addition to the definition, the WHO has standardised the naming of the syndrome. Since 1998, it has recommended the use of the name "metabolic syndrome", which is currently the most widely used name.
What other names for metabolic syndrome have been commonly used in practice?
These were names such as:
- Pluri-metabolic syndrome
- Cardiac dysmetabolic syndrome
- The death quartet
- Obesity syndrome
- Insulin resistance syndrome
- 5H syndrome
- Syndrome X
Causes
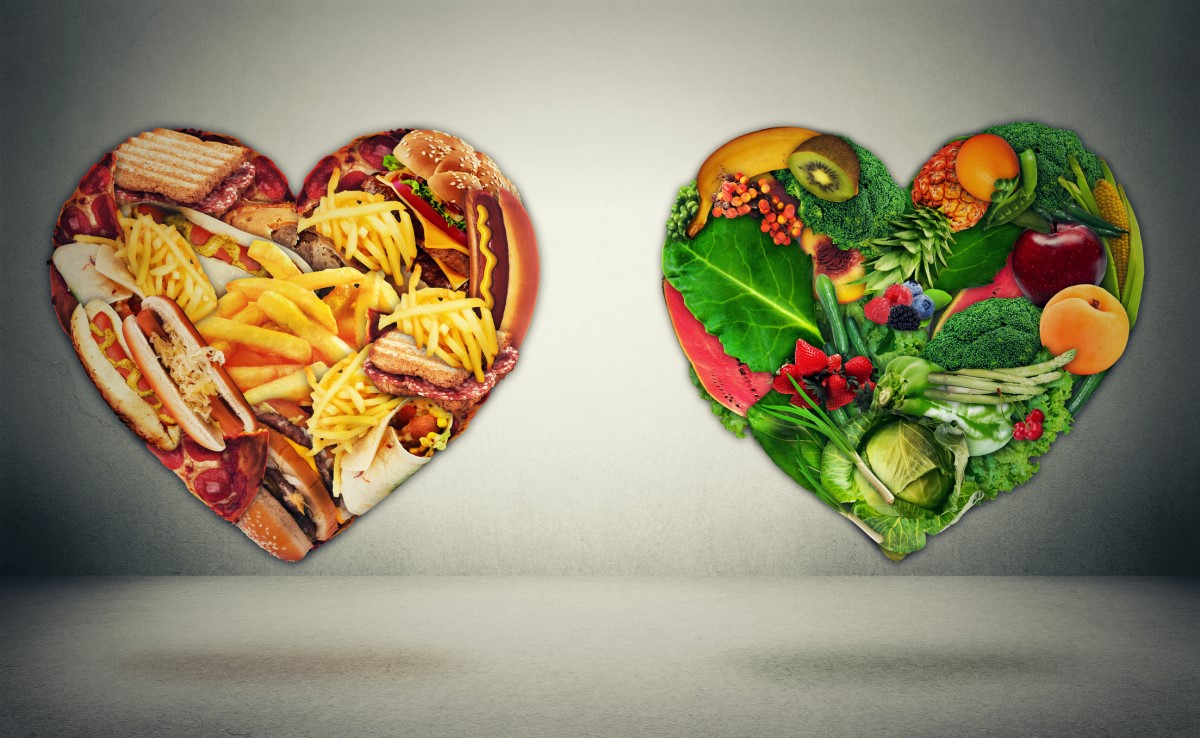
Many literature data indicate that the development of metabolic syndrome in the body is primarily related to overweight, obesity and inactive lifestyle.
Poor or inappropriate lifestyles are now becoming a global problem, whether we are talking about diet or daily physical activity.
Increased intake of particularly high-calorie foods that are also low in protein, reduced physical activity, sedentary lifestyles or passive leisure activities have a significant impact on the overall health of the population.
There are increasing numbers of overweight people and even obese people.
Overweight/obesity as a risk factor for metabolic syndrome
The way and especially the place where excessive fat storage occurs is important for the development of metabolic syndrome.
In this case, the risk area for fat deposition is the upper half of the body, i.e. the waist. The fat accumulated in this part of the body causes the typical apple or pear shape.
Excessive fat deposition in the body (adiposity in the technical language) contributes to metabolic syndrome in two ways.
The first way is that adipose tissue is considered an active organ in addition to an energy store. It produces fat hormones (leptin) and chemicals that induce an inflammatory response (inflammatory cytokines).
Leptin is thought to induce a feeling of satiety in the body and reduce fat stores by promoting energy expenditure.
In obesity, there is more fat tissue. Therefore, a relatively large amount of leptin is produced. The body reacts differently to this amount of hormone than we would expect. It becomes resistant, i.e. resistant to its action, and breaks down the accumulated fat to a lesser extent.
In parallel with the pro-inflammatory effect of cytokines, it thus contributes to the deposition of fats in the walls of blood vessels, which leads to atherosclerosis and also to an increase in blood pressure.
The second way in which adiposity contributes to the development of metabolic syndrome is by inducing insulin resistance. To understand this mechanism, it is necessary to explain the concept of insulin resistance.
Insulin resistance as a risk factor for metabolic syndrome
Insulin resistance refers to a reduced sensitivity to tissue and insulin cells. Insulin is a hormone produced in the pancreas. It is supposed to help glucose taken from the diet move into the cells where it is used for energy production.
In this case, the skeletal muscle cells are resistant to the action of the attached insulin and do not take up glucose into their interior. It accumulates in the bloodstream.
The body compensates for this disturbance by overproducing insulin to reduce the elevated glucose levels. However, excessive insulin production causes a number of other side effects, such as increased blood pressure or disturbed blood fat levels.
This mechanism contributes to the cells to develop metabolic syndrome and is one of its most common causes.
Increased adiposity (excessive fat storage) is also likely to contribute to insulin resistance.
This mechanism is explained as follows.
Adiposity causes an increase in free fatty acids.
These acids counteract the process of glucose utilization in skeletal cells by interfering with the action of insulin.
Subsequently, cellular resistance to insulin develops.
Adiposity, together with insulin resistance and excessive insulin levels in the body, are now considered to be the primary causes of metabolic syndrome.
Other possible causes of metabolic syndrome
In addition to the above, disorders of blood lipid levels (in particular elevated triacylglycerols and reduced HDL cholesterol) may also be a cause of metabolic syndrome. In this case, the mechanism of action is to increase the breakdown of body fat.
Other causes are high blood pressure (mechanism unexplained), genetic factors, race, sex and, last but not least, age.
As age increases, so does the risk of metabolic syndrome.
One of the hypotheses for the development of metabolic syndrome is the so-called 'thrifty genotype hypothesis'. Thrifty genes have been used especially in periods of energy shortage (e.g. wars, famine). The genes were designed to store energy from food supply in a highly efficient manner. However, in the current population, the role of these genes is rather disadvantageous. The daily energy intake of an individual is much higher, and thus energy storage in the form of fat stores increases.
Other causes potentially contributing to metabolic syndrome are currently under study, such as fatty liver, polycystic ovary syndrome, gallstones or breathing problems during sleep (sleep apnoea).
People at risk
From the above information, we can briefly summarise the groups of people who are at higher risk of developing metabolic syndrome.
- People who are overweight or obese, with excessive fat accumulation, especially around the waist
- People with an inactive lifestyle (little physical activity, sedentary lifestyle)
- People who have developed insulin resistance
- People with diabetes or a family history of diabetes
- Certain races or ethnic groups. For example, Hispanics have the highest risk, followed by whites and then blacks
- Specific gender. Women have a higher risk of developing the syndrome than men.
- People taking certain medications, such as medications that affect weight, blood pressure, cholesterol, blood fat levels, etc.
Prevention
In addition to the treatment itself, appropriate prevention has been proven in practice.
The most basic preventive measure that can be taken to prevent the onset or worsening of symptoms and manifestations is to modify the lifestyle that has been adopted.
Based on many clinical studies, it can be argued that any intervention on the individual components of the metabolic syndrome has a positive impact on overall morbidity and mortality.
Read also: How to prevent cardiovascular disease?
Regular check-ups with a doctor are also important, during which cholesterol, fat and blood sugar levels are monitored, as well as blood pressure.
An overview of basic actions to reduce the risk of developing or worsening metabolic syndrome (table)
| Preventive measures to prevent the development of metabolic syndrome |
|
|
|
|
|
|
The same lifestyle modification procedures are subsequently applied in the non-pharmacological treatment of metabolic syndrome.
In addition to individual efforts, preventive measures can include more comprehensive measures such as spatial plans to promote active lifestyles, subsidies for healthy foods, promotion of healthy eating habits and education of the population in healthy eating, limiting advertising of unhealthy foods, etc.
A higher prevalence of metabolic syndrome is associated with populations living in cities and in developed countries. This prevalence is mainly due to a higher consumption of high-calorie foods, together with a lack of physical activity and a sedentary lifestyle.
Symptoms
Their existence is proven by a series of clinical tests (blood tests).
The most typical and visible sign of the possible presence of the syndrome is a wide waist circumference caused by accumulated subcutaneous fat.
If an individual is overweight or obese, the most common associated symptoms are:
- breathing problems
- increased sweating
- night-time snoring
- difficulty moving around and performing physical activities
- fatigue
- joint and spinal pain
More severe forms of raised blood pressure may manifest
- headache
- dizziness
- difficulty breathing
- nosebleeds
In the case of excessively elevated blood glucose levels
- marked thirst
- increased urine output (especially at night)
- fatigue
- blurred vision
However, these symptoms are characteristic of a long-term increase in blood glucose. They do not occur with a short-term increase. In the case of long-term elevated glucose levels, advanced diabetes is already considered, which is considered a negative consequence of the metabolic syndrome.
Summary of symptoms mentioned:
- Wide waist circumference
- Overweight
- Obesity
- Breathing problems
- Increased sweating
- Snoring at night
- Difficulty moving around and doing physical activities
- Fatigue
- Joint and spinal pain
- High blood pressure
- Headache
- Dizziness
- Shortness of breath
- Nosebleeds
- Increased blood glucose levels
- Significant thirst
- Increased urine output (especially at night)
- Blurred vision
- Increased cholesterol levels in the blood
- Chest pain
- Formation of blood clots
- Fatty liver associated with inflammation
Diagnostics
The presence of five pathological conditions is assessed - elevated blood pressure, high blood sugar, excessive body fat in the waist area, elevated cholesterol and triacylglycerol levels in the blood.
For a patient to be diagnosed with metabolic syndrome, at least three of these disorders, or more, must be present.
There are currently several approaches to the diagnosis of the syndrome that have been recommended by health care organisations. These approaches differ in particular as to which is considered to be the primary cause of the metabolic syndrome.
In addition, they differ in the cut-off values of certain biochemical parameters that are determined in the diagnosis and that indicate a disease state.
Overview of the diagnostic criteria for metabolic syndrome recommended by health organisations (table)
| WHO recommendations (1999) | |
| Presence of insulin resistance or a fasting glucose level >6.1 mmol/l (110 mg/dl) concurrent with any two or more of the following conditions: | |
| HDL cholesterol | Men: <0.9 mmol/l (35 mg/dl) Women: <1.0 mmol/l (40 mg/dl) |
| Triacylglycerols | >1.7 mmol/l (150 mg/dl) |
| Waist/hip circumference ratio | Men: >0.9 Women: >0.85 |
| Body mass index (BMI) | >30 kg/m2 |
| Blood pressure | >140/90 mmHg |
| National Cholesterol Education Program (National Cholesterol Education Program, Adult Treatment Panel III, 2005) | |
| Presence of any three or more of the following conditions: | |
| Fasting glucose | >5.6 mmol/l (100 mg/dl) or ongoing treatment with blood glucose-lowering medications |
| HDL cholesterol | Men: <1.0 mmol/l (40 mg/dl) Women: <1.3 mmol/l (50 mg/dl) or ongoing treatment with cholesterol-lowering drugs |
| Triacylglycerols | > 1.7 mmol/l (150 mg/dl) or ongoing treatment with medication to lower blood fats |
| Waist circumference | Men: >102 cm Women: >88 cm |
| Blood pressure | >130/85 mmHg or ongoing treatment with blood pressure lowering medication |
| Recommendations of the International Diabetes Federation (2006) | |
| Waist circumference >94 cm in men or >80 cm in women concomitant with any two or more of the following conditions: | |
| Fasting glucose | >5.6 mmol/l (100 mg/dl) Or diagnosed diabetes |
| HDL cholesterol | Men: <1.0 mmol/l (40 mg/dl) Women: <1.3 mmol/l (50 mg/dl) Or ongoing treatment with cholesterol-lowering drugs |
| Triacylglycerols | >1.7 mmol/l (150 mg/dl) or ongoing treatment with medication to lower blood fats |
| Blood pressure | >130/85 mmHg or ongoing treatment with blood pressure lowering medication |

Course
The pathological disturbances characteristic of the metabolic syndrome arise gradually. They must be continuous and present over a long period of time in order to manifest themselves visibly in the body.
The disorders may develop independently of each other, but in most cases they build on each other. One disorder builds on another, pre-existing disorder. This is similar to a chain reaction.
We only speak of a metabolic syndrome when an individual has at least three or more of these disorders in parallel.
In metabolic syndrome, we do not observe typical, outwardly visible symptoms that would point to a possible problem.
Symptoms are usually only noticeable when there is a significant worsening of one of the components of the syndrome, such as excessively high blood pressure or excessively high glucose levels.
The onset and subsequent progression of metabolic syndrome is closely related to an individual's lifestyle. Poor lifestyle combined with unbalanced food intake and lack of exercise is causing an increasing incidence of weight problems.
A tell-tale sign that may indicate the risk of metabolic syndrome is excessive fat concentrated mainly around the patient's waist.
Although most of the components of metabolic syndrome are not apparent at first glance, their early recognition is a critical factor in maintaining a healthy and functioning body.
Therefore, it is not a good idea to forget about regular preventive check-ups with a doctor, which can help to detect a problem that is invisible at first glance.
Metabolic syndrome in children
The incidence of metabolic syndrome is not exceptional in the paediatric population. As the number of overweight (even obese) children continues to rise, an increased incidence of metabolic changes is observed.
The primary cause of obesity in children is the same as in adults - a disparity between energy intake and energy expenditure.
Obesity in childhood, or excess adipose tissue in relation to other organs, causes fluctuations in both fat and sugar metabolism.
These fluctuations, together with obesity and associated elevated blood pressure, lead to the development of metabolic syndrome in children.
The methods of diagnosis of the syndrome in the paediatric population are similar to those in adults, with differences in the threshold values of some biochemical parameters.
Currently, it is recommended to diagnose the syndrome according to the criteria of the International Diabetes Federation, which considers obesity as the primary cause of the onset and development of metabolic syndrome in children.
Diagnosis is only made in children aged 10 to 16 years. Diagnosis is not recommended in younger children. Patients over 16 years of age are already subject to the same criteria as adults.
Overview of the diagnostic criteria for metabolic syndrome in children (table)
| Recommendations of the International Diabetes Federation | |
| Central obesity - waist circumference ≥90 cm concomitant with any two or more of the following conditions: | |
| Fasting glucose | ≥5.6 mmol/l or ongoing treatment with blood glucose-lowering medications |
| HDL cholesterol | ≤1.03 mmol/l |
| Triacylglycerols | ≥1.7 mmol/l |
| Blood pressure | ≥130/85 mmHg |
How much energy do we consume in our diet:
Calorie tables: what are the nutritional/nutrient values of foods?
How it is treated: Metabolic syndrome
Treatment: for metabolic syndrome, a change in lifestyle and only then a cure
Show moreExpert debate on the causes and consequences of the disease - video
Metabolic syndrome is treated by
Metabolic syndrome is examined by
Other names
Interesting resources
Related










