How is coxarthrosis treated? Medication, exercise to after surgery of the joint
Why start treatment for coxarthrosis as soon as possible?
Treatment of arthritis must be started at the first signs and slow or stop the degenerative process in the joint. If left untreated and the body's signals are ignored, the destructive process in the hip joint can develop accelerated.
In addition to the pain itself and the limitation of movement in the joint, complex muscular imbalances can develop in a person's musculoskeletal system.
In pain, analgesic walking is typical. This refers to walking that "spares" the damaged joint and puts more stress on the other.
Prolonged overloading of the opposite hip joint can lead to rapid wear and tear and arthrosis in the other, healthy joint.
Misalignment of the back and an oblique pelvic position are present, which in turn affects the posture of the trunk, shoulders and head.
After a certain period of time, the appearance of muscle pain is possible even in the outermost parts of the body.

Treatment of coxarthrosis
Treatment of hip arthrosis is divided into conservative and surgical.
The main goal of arthrosis treatment is to delay invasive treatment, specifically artificial hip replacement. It always depends on the patient's objective and subjective symptoms and the agreement with the doctor.
Usually, conservative treatment is applied. Subsequently, the results are evaluated to determine the appropriateness and necessity of surgery. If the patient's pain is advanced and acute, joint replacement (endoprosthesis) is recommended immediately.
Conservative treatment
Conservative treatment is aimed at eliminating pain, increasing joint mobility, strengthening weakened muscles, relaxing overworked muscles, weight control, modifying physical activity, and teaching proper ergonomics for work and normal daily activities.
The main representatives of pharmacological treatment are analgesics, non-steroidal anti-inflammatory drugs and chondroprotective agents.
The treatment is based on effective local nutrition of the joint in the form of hyaluronic acid, collagen and other chondroprotective agents. The doctor administers painless injections directly into the inner side of the joint capsule of the damaged joint.
Conservative treatment involves passive therapy using the positive effects of physical therapy such as electrotherapy, phototherapy, ultrasound, thermotherapy or hydrotherapy.
The choice of a particular type of therapy always depends on the desired effect, which is usually analgesic (pain-relieving) and healing (regenerative).
Physiotherapy is an integral part of arthritis therapy. Rehabilitation is prescribed by the doctor both preventively and in the pre- and post-operative phase of treatment.
Coxarthrosis is one of the most common orthopaedic diagnoses encountered by physiotherapists in outpatient clinics, hospitals and rehabilitation institutes.
In joint sessions, the physiotherapist relaxes and mobilises the patient's hip, sacroiliac joint and joints of the cervical spine. Using soft and manual techniques, he or she influences and eliminates muscle spasms.
Practices exercises with the patient, especially to strengthen and stabilize the gluteal muscles and the muscles near the hip joint.
Coxarthrosis and exercise
The physiotherapist selects specific exercises according to the goal of therapy and the patient's health condition. Exercises vary in the preventive phase, the pre-operative phase and the post-operative phase.
After surgery, the patient observes certain movement principles and restrictions (no crossing of legs, low sitting, high load on the hip joint, excessive rotation, etc.).
The most commonly used exercise is the glute bridge, which is used to strengthen the gluteal muscles.
The patient lies with his/her whole back and head on a soft mat with the legs bent at the knees. There is no space between the mat and the spine. The legs are glued to the mat along their entire length and the arms are loosely placed next to the body. Regular diaphragmatic and abdominal breathing is observed.
With an exhalation, the patient gradually peels the vertebrae off the mat vertebra by vertebra and raises the pelvis to the ceiling. He contracts and engages the gluteal muscles.
The patient remains in the higher position. He inhales and exhales several times into the ribs, but does not allow contraction of the gluteal muscles.
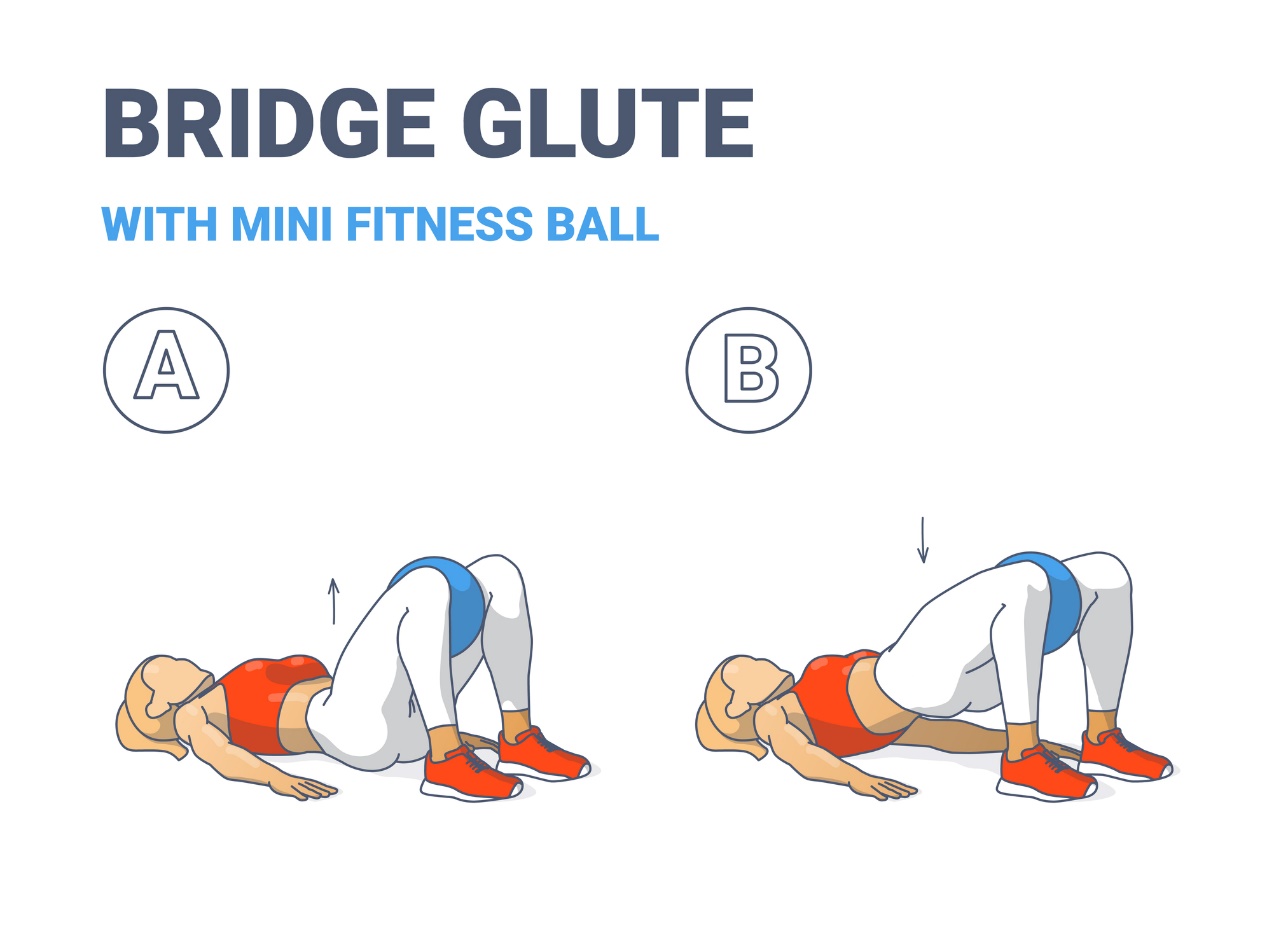
Then, with an exhalation, the patient slowly and smoothly lies back down on the mat in the starting position and relaxes the gluteal muscles. For the safety of the exercise, the patient may place a soft gymnastic ball or cushion between the thighs to prevent excessive adduction and crossing of the legs.
A variation of this exercise to strengthen both the gluteal muscles and the abductors of the thigh (unweighted) is to use the upper glute bridge position, whereby the knees are simultaneously pulled apart (frog) as the gluteal region contracts.
We then smoothly bring the knees back together to the level of the hip joints. It is advisable to practice against slight resistance (resistance cloth rubber or the therapist's hands slightly resisting the movement of the practitioner).
Again, the shoulder blades remain glued to the mat throughout the exercise. Attention is paid to diaphragmatic abdominal breathing (breathing to the sides of the lower ribs).
Consultation with a therapist is recommended to make the therapy more effective and to avoid mistakes during the exercises. The therapist will prepare exercises tailored to the patient, his/her diagnosis and the goal of the therapy.
Biological treatment
Biological treatment is the newest type of conservative treatment. It is not often used due to its cost.
It involves taking the body's own stem cells from fat, which are injected directly into the damaged joint. These have the ability to repair, regenerate cells and tissues in the body.
Patients with grade I and II arthritis subjectively rated their improvement in health in questionnaires. Approximately 65% of patients experienced a reduction in pain and some improvement in mobility of the damaged joint 6 months after the procedure.
The treatment is more effective and has a more lasting effect the more it is applied at a lower stage of arthrosis.
Due to advances in development and medicine, it is believed that biological therapy may be the most effective form of osteoarthritis therapy in the future.
Hip replacement
Endoprosthesis, a hip replacement, is indicated when the condition has not improved with conservative treatment. It is often recommended for higher degrees of arthritis and severe pain.
The most common reason for hip replacement is coxarthrosis.
Endoprostheses are made of titanium, cobalt or chromium. These materials have a long service life. There are two types of replacements, namely partial and total.
In partial replacement, the damaged part of the joint is replaced. In total replacement, both parts of the joint surfaces are replaced.
Modern times offer a large selection of implants. This allows doctors to choose an adequate type of endoprosthesis for each type of disability.
Implants are divided into:
- cemented
- uncemented
- hybrid
A cemented replacement using bone cement is smoother on the surface and fully loadable soon after surgery. The disadvantage is the eventual replacement. The surgeon would subsequently have a more difficult access.
It is therefore mainly used in elderly and inactive patients.
An uncemented prosthesis, on the other hand, is rough on the surface and its stable anchorage occurs gradually. The disadvantage is the impossibility of full loading soon after surgery.
However, it is an easy surgical option for possible replacement in the future. It is suitable for younger and more active patients.
In hybrid replacements, each bone component is individually fixed in a different way.
Recovery and complications
In most cases, recovery after hip arthroplasty is easy and painless. Both the patient and the therapist try to ensure that the "new" joint can be fully used as soon as possible after surgery.
The patient may experience soreness in the muscles around the hip joint in the sense of muscle imbalance. However, this can be corrected relatively quickly with proper rehabilitation. The body and the surrounding structures of the joint gradually become accustomed to the new joint.
Possible complications are associated with general and local anaesthesia, as with other surgical procedures. Local complications are minimal but possible. They may include postoperative dislocation of the endoprosthesis, infection or neuromuscular disorders of the operated area.
Rehabilitation begins immediately on the day of surgery. It is carried out with the participation of physiotherapists using rehabilitation aids such as motor splints, treadmills or overballs and gymnastic balls.
While standing, the patient is trained to walk on two French canes on a flat surface. Once this is mastered, the distance is gradually extended and the patient learns to walk on stairs.
For the first 6 weeks after the operation (of which approximately 2 weeks in hospital) the process of adaptation and healing of the operated joint takes place. During this time the patient must not fully load the limb and should walk with the help of crutches.
By slowly loading the operated side, the patient gets rid of the crutches. The patient exercises with the physiotherapist from the day of surgery in the hospital and subsequently during meetings in the rehabilitation clinic.
The result is a full return to life.











