- Ortel, TL; Neumann, I; Ageno, W; et al. (13 October 2020). "American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism". Blood Advances. 4 (19): 4693–4738. doi:10.1182/bloodadvances.2020001830. PMC 7556153. PMID 33007077.
- Heit JA, Spencer FA, White RH (January 2016). "The epidemiology of venous thromboembolism". Journal of Thrombosis and Thrombolysis. 41 (1): 3–14. doi:10.1007/s11239-015-1311-6. PMC 4715842. PMID 26780736.
- Abbattista M, Capecchi M, Martinelli I (January 2020). "Treatment of unusual thrombotic manifestations". Blood. 135 (5): 326–334. doi:10.1182/blood.2019000918. PMID 31917405.
- National Clinical Guideline Centre – Acute and Chronic Conditions (UK) (2010). "Venous Thromboembolism: Reducing the Risk of Venous Thromboembolism (Deep Vein Thrombosis and Pulmonary Embolism) in Patients Admitted to Hospital". PMID 23346611.
- Shatzel, Joseph J.; O'Donnell, Matthew; Olson, Sven R.; Kearney, Matthew R.; Daughety, Molly M.; Hum, Justine; Nguyen, Khanh P.; DeLoughery, Thomas G. (January 2019). "Venous thrombosis in unusual sites: A practical review for the hematologist". European Journal of Haematology. 102 (1): 53–62. doi:10.1111/ejh.13177. ISSN 0902-4441. PMID 30267448.
- Windecker, Stephan; Stortecky, Stefan; Meier, Bernhard (July 2014). "Paradoxical Embolism". Journal of the American College of Cardiology. 64 (4): 403–415. doi:10.1016/j.jacc.2014.04.063. PMID 25060377.
- Martinelli I, Bucciarelli P, Mannucci PM (2010). "Thrombotic risk factors: basic pathophysiology". Crit Care Med. 38 (suppl 2): S3–9. doi:10.1097/CCM.0b013e3181c9cbd9. PMID 20083911. S2CID 34486553.
- Bovill EG, van der Vliet A (2011). "Venous valvular stasis-associated hypoxia and thrombosis: what is the link?". Annu Rev Physiol. 73: 527–45. doi:10.1146/annurev-physiol-012110-142305. PMID 21034220.
- Rosendaal FR, Reitsma PH (2009). "Genetics of venous thrombosis". J. Thromb. Haemost. 7 (suppl 1): 301–4. doi:10.1111/j.1538-7836.2009.03394.x. PMID 19630821. S2CID 27104496.
- Khan NR, Patel PG, Sharpe JP, Lee SL, Sorenson J (2018). "Chemical venous thromboembolism prophylaxis in neurosurgical patients: an updated systematic review and meta-analysis". Journal of Neurosurgery. 129 (4): 906–915. doi:10.3171/2017.2.JNS162040. PMID 29192859. S2CID 37464528.
Patients requiring cranial and spinal surgery present a unique situation of elevated risk for VTE but also high risk for disastrous outcomes should bleeding complications occur in eloquent areas of the brain or spinal cord.

- Stein PD, Beemath A, Meyers FA, et al. (2006). "Incidence of venous thromboembolism in patients hospitalized with cancer". Am J Med. 119 (1): 60–8. doi:10.1016/j.amjmed.2005.06.058. PMID 16431186.
- Jackson E, Curtis KM, Gaffield ME (2011). "Risk of venous thromboembolism during the postpartum period: a systematic review". Obstet Gynecol. 117 (3): 691–703. doi:10.1097/AOG.0b013e31820ce2db. PMID 21343773. S2CID 12561.
- Varga EA, Kujovich JL (2012). "Management of inherited thrombophilia: guide for genetics professionals". Clin Genet. 81 (1): 7–17. doi:10.1111/j.1399-0004.2011.01746.x. PMID 21707594. S2CID 9305488.
- Turpie AGG (March 2008). "Deep Venous Thrombosis". The Merck's Manuals Online Medical Library. Merck.
- Beyer-Westendorf J, Bauersachs R, Hach-Wunderle V, Zotz RB, Rott H. Sex hormones and venous thromboembolism - from contraception to hormone replacement therapy. Vasa. 2018
Thromboembolic disease: origin and how it relates to pulmonary embolism
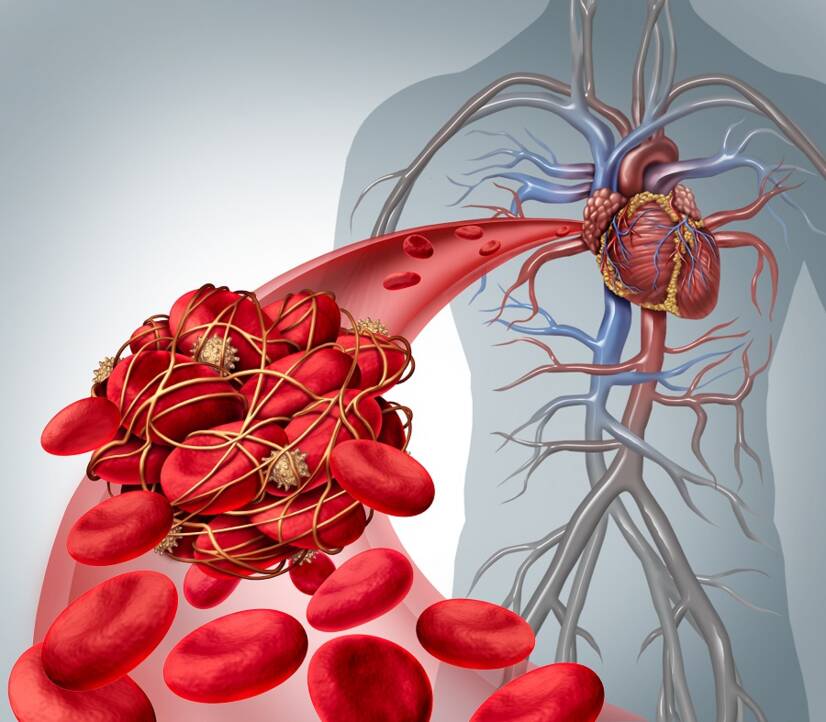
Photo source: Getty images
Most common symptoms
- Chest pain
- Leg Pain
- Spirituality
- Head spinning
- Malaise
- Blue leather
- Sweating
- Low blood pressure
- Swelling of the limbs
- Feeling of heavy legs
- Disorders of consciousness
- Pressure on the chest
- Fatigue
- Coughing up blood
- High blood pressure
- Accelerated heart rate
- Heart enlargement
Show more symptoms ᐯ
Treatment of thromboembolic disease: medications and invasive methods
Show moreThromboembolic disease is treated by
Thromboembolic disease is examined by
Other names
thromboembolic disease, thromboembolism, acute thromboembolic disease, chronic thromboembolic disease, thromboembolic state, venous thromboembolic disease










