Pulmonary embolism: causes, symptoms, probability testing, and treatment
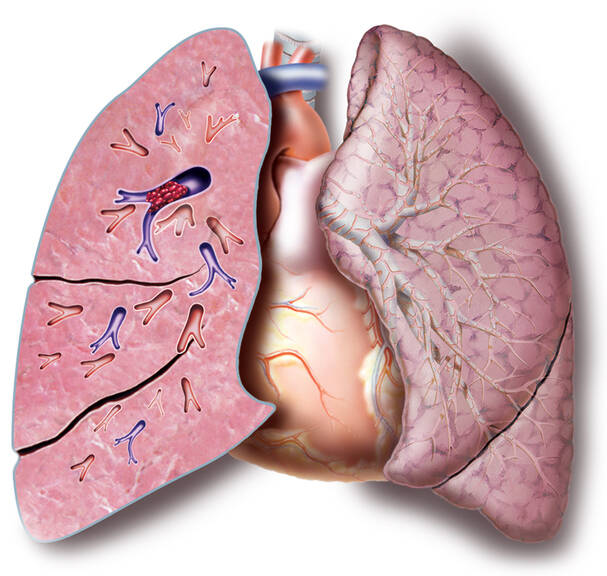
Pulmonary embolism (PE) is an acute condition in which blood vessels in the lungs become clogged. The most common cause is thromboembolic disease. A blood clot is released and travels through the vessels as an embolus. It clogs vessels. The massive form of PE is life-threatening.
Most common symptoms
- Sweating
- Chest pain
- Painful Breathing
- Spirituality
- Fever
- Increased body temperature
- Pressure on the chest
- Fatigue
- Anxiety
- Damp cough
- Vomiting
- Coughing up blood
- Confusion
- Accelerated heart rate
- Heart enlargement
Characteristics
Pulmonary embolism is an acute (i.e. having a sudden, recent onset) condition that blocks a pulmonary artery. The most common cause of vascular occlusion is a thromboembolic disease. A thrombus, also called a blood clot, is released and travels as an embolus through the bloodstream. It comes mainly from the vessels of the lower limbs and the pelvis.
A thromboembolic disease, or venous thromboembolism (VTE), occurs mainly as a result of immobilisation (prolonged sitting or bed rest) or a lower limb.
Postoperative conditions in particular are a risk. For example, after replacing the hip or knee joint, but also when the lower limb is immobilized with a splint, plaster in the event of a fracture.
Of course, there are other diseases that can cause thrombosis, such as phlebothrombosis of the lower extremities. In addition to blood clots, vascular occlusion is also caused by other material.
An obstruction in the pulmonary vessels can be caused by:
- blood clot, or thrombus, called an embolus after it is released into the bloodstream
- air
- fat
- amniotic fluid
- tumour
Pulmonary embolism is the third most common cardiovascular disease. Ranking below it is hypertension and coronary heart disease (CHD). It is also a major risk factor and cause of morbidity and death. The mortality rate of untreated pulmonary embolism is reported to be up to 30%.
Early diagnosis and prompt treatment reduce this percentage to 2 to 8 percent risk.
In the past, the classification of pulmonary embolism used to be based on the extent of vascular occlusion. Today, pulmonary embolism is determined by risk of early mortality. Both classifications are listed in the table.
FAQ:What is it, why does it arise and how does it manifest itself?How is it identified and treated?What are the complications and risks?Find out by reading the article...
Table: classification of pulmonary embolism
| Risk | Risk of death in percentage | Description |
| High-risk | over 15 % |
shock low blood pressure |
| Intermediary risk | 3 - 15 % | impaired right ventricular function markers of heart muscle damage |
| Low-risk | less than 1 % | without impairing right ventricular function without deteriorating hemodynamics without damaging the heart muscle |
| Grade | former classification of pulmonary embolism determines the extent of the obstruction, i.e. the occlusion of the vessel, in percent | |
| Minor | below 25 % | |
| Submassive | 25 - 50 % | |
| Massive | 51 - 65 % | |
| Fulminant | over 66 % | |
What is a thromboembolic disease?
Thromboembolic disease is a disease process that results from the presence of a thrombus or embolus in the blood vessels. It has two subunits, the pulmonary embolism and deep vein thrombosis. Deep vein thrombosis occurs in the upper or lower limbs, or in the pelvis.
The most common cause of embolization is deep vein thrombosis of the lower limbs. Another area is thrombosis of the vessels of the pelvis, kidneys, or during the inferior vena cava. A blood clot, or embolus, can also cause blood vessels to close in the abdomen or upper limb.
Stroke is a serious condition.
Learn more:
Thromboembolic disease
Stroke
Pulmonary embolism is a life-threatening condition. Its most common cause is deep thrombosis of the lower limbs. The embolus, which forms in the vessels of the lower limbs, travels in the bloodstream and clogs the pulmonary arteries, or branches of the pulmonary artery, is also referred to as the lungs.
The most frequent origin of a thrombus is the vessels of the lower limbs.
However, it can form in the vessels of the upper limbs or in the right heart. A blood clot can form in the altered vessel, as is the case with varicose veins.
Causes
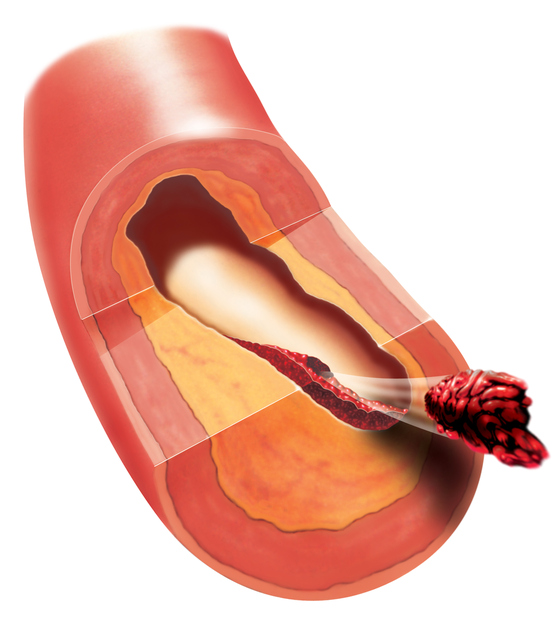
The cause of pulmonary embolization is mainly thromboembolic disease.
It represents up to 85% of embolisations. However, there are other obstructions that may be behind the occlusion of the vessel: adipose tissue, air, amniotic fluid or tumour cells.
In the case of thrombosis, and therefore in the case of lung embolism, there are predisposing factors that cause problems, especially when combined. They are also referred to as the Virchow's Triad. Detection of the presence of risk factors is crucial in determining subsequent preventive measures.
In addition, there are common risk factors for lung embolism. They can be innate or acquired.
Thrombosis occurs as a combination of several factors, also referred to as the Virchow's Triad:
- change in the coagulation mechanism, i.e. blood clotting
- disruption of the internal vascular mucosa, i.e. the endothelium
- slower blood flow
- vascular change as in varicose veins, inflammation
- in cardiac arrhythmia
- the current state of the fibrinolytic system is also important
The most common risk factors to cause a thromboembolic disease:
- advanced age
- genetic and familial predisposition
- increased levels of coagulation factors
- decreased levels of proteins C, S, or antithrombin III
- antiphospholipid syndrome
- dehydration
- vascular inflammation
- Lower limb varicose veins
- blood stasis in the lower limbs, i.e. affected backflow
- long flight
- standing for a long time
- sitting for a long time
- long drive
- more than 4 hours
- smoking
- obesity
- lack of movement, immobilisation
- complete immobilisation for more than 3 days
- partial immobilisation of the lower limb with a splint, plaster
- surgery
- especially major surgeries
- in the abdominal cavity
- joint replacements of the lumbar or knee joint, i.e. total endoprosthesis (TEP)
- artificial valve prostheses, stents
- central venous catheter
- hormonal changes
- hormonal contraceptives
- pregnancy, especially in the 2nd and 3rd trimesters
- postpartum (or postnatal) period
- tumourous disease
- ulcerative colitis
- infection and sepsis
- injuries, burns, polytrauma
- past recovery from embolism, thrombosis, stroke or heart attack
- drug abuse
A blood clot, or a thromboembolus, or other material travels through the blood vessels until it creates a barrier to blood flow, an obstruction in the pulmonary stream. The onset of difficulties and the image of a massive pulmonary embolism in a healthy person are formed by the closure of 50% of the pulmonary vessels.
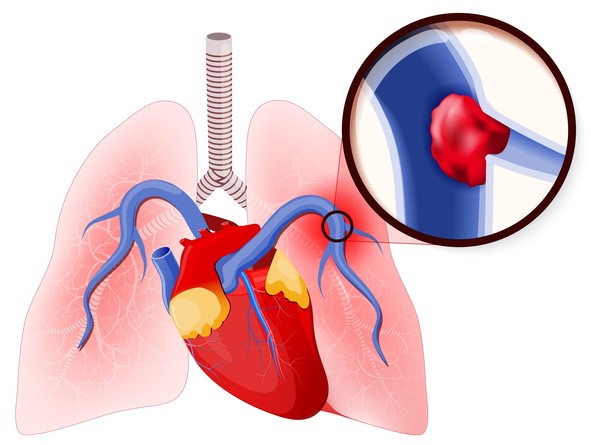
The embolus creates an obstacle in branches of the pulmonary artery. Depending on the extent and restriction of the blood flow, there is a disruption of the pulmonary circulation. Impaired pulmonary circulation is due to a reduction in venous return to the left heart.
The blood returns to a lesser extent from the right side of the bloodstream to the left heart, which causes reduced pressure in the major circulatory system and increased pressure in the pulmonary artery (pulmonary hypertension) and in the right heart. This is the cause of overloading the right heart.
If the extent of embolisation is large, such as when obstructing a pulmonary artery strain, the patient may suddenly die. If the embolisations are recurrent but small, chronic right heart failure, pulmonary hypertension, and later right ventricular dilatation occur.
Learn more: Enlargement and dilation of the heart
Embolisation occurs mainly due to deep venous thrombosis of the lower extremities. There is a proximal and a distal form. The proximal form is located above the knee, mainly from femoral (44.1%) and iliofemoral thrombosis (13.5%). Overall, the risk for embolisation us up to 50% if left untreated.
For example, take a distal vessel from the lower leg with thrombosis in the calf area. The risk is 5-25% in case of non-treatment. In about 5.1% of cases, the source of embolization is the right heart.
As many as 33.9% of postmortem examinations showed unknown sources of embolisation.
The blood clot adheres to the vessel wall and some thrombi hold on to it better. Others are unstable and in most cases are released into the bloodstream after mechanical pressure, for example due to coughing, during defecation, vomiting, or standing up too quickly.
Symptoms
The symptoms of pulmonary embolism depend on the extent of the damage to the vessel branches.
When the vessel is clogged, the blood flow in the affected part of the lungs is disrupted. Moreover, a pulmonary tissue infarction can occur if the vascular supply to the lungs is impaired (less than 10% of cases).
In some cases, it can also be asymptomatic. The overall clinical picture depends on several factors:
- extent of the obstruction
- size of the embolus
- duration of onset
- condition of the cardiovascular system
Typical symptoms of pulmonary embolism are difficulty breathing and rapid breathing. Chest pain may be an associated problem. Tje heart rate is elevated. Other associated symptoms that can lead to a diagnosis include cough, coughing up blood, and collapsing.
Table: percentage of typical symptoms in pulmonary embolism
| Symptom | Percentage | Description |
| dyspnoea | 82 | difficulty in breathing abrupt onset it also arises at rest, without prior overload the percentage is indicated in up to 95 cases |
| tachypnoea | 60 | unusually rapid breathing over 20 breaths per minute in all its forms |
| chest pain | 49 |
may resemble a myocardial infarction or has a pleural character
|
| increased heart rate | 40 | tachycardia accelerated pulse / heart rate above 100 per minute |
| cough | 20 | |
| collapse | 14 | syncope, or fainting, temporary loss of consciousness may be the first manifestation of the disease |
| hemoptysis | 7 | coughing up blood |
In case of massive pulmonary embolism, the hemodynamics are impaired, and blood pressure in the lungs increases. He is a burden to the true heart. The right heart is failing. As a result of the reduced backflow of blood to the left heart, the circulating blood pressure drops. The result is cardiogenic shock. The risk of a damaged blood supply to the heart is a heart attack.
Learn more: First aid in heart attack
The massive form of pulmonary embolism presents with symptoms such as:
- increased sweating
- pallor
- low blood pressure
- tachycardia
- rhythm disorders - gallop rhythm
- pulmonary hypertension
- acute dilatation of the right ventricle
- increased central venous return, which can be seen in the increased filling of the jugular veins
- disorder of consciousness, collapse
Untreated massive pulmonary embolism has a high risk of death.
Treated embolism has a 20 percent risk of death.
Sudden death occurs in approximately 10% of cases.
Other symptoms may cause the skin to turn bluish, i.e. cyanosis. It can be present at the periphery first, but also centrally later on. The sufferer may be show signs of fear of impending death.
Hiccups, also known as singultus, can also be associated. The affected person may have an upset stomach or vomit. In the chronic type, the patient may present with swelling of the lower limbs, increased fatigue and general weakness. Collapse may be the first sign of illness. Ther emay be bladder and bowel incontinence.
Submassive embolism presents with less severe problems. But it is also characterised by shortness of breath or pain behind the sternum. There are no signs of shock in this type. Vascular occlusion is less than 50%.
Another form is successive pulmonary embolism characterised by recurrent embolisation of smaller clots. It is also referred to as the relapsing form. Its incidence is reported to be about 29%. It is often mistaken for other lung or heart disease.
Symptoms of pulmonary embolism:
- sudden shortness of breath
- chest pain
- cough
- coughing up blood
- palor
- sweating
- fear of impending death
- fainting
- rapid breathing
- increased pulse
- low blood pressure
- cardiogenic shock
- cyanosis
- dizziness
- deep vein thrombosis in the legs
- temperature above 38,5 °C
Diagnostics
The diagnosis of pulmonary embolism is easier due to the disease's typical course. However, that might not be the case every time. Sometimes diagnostic errors are made, confusing embolism with another disease, e.g. bronchopneumonia, myocardial infarction, or heart failure.
Suspicion of diagnosis must be made in the event of difficulties together with the presence of phlebothrombosis and positivity of elevated D-dimers (more than 500 units). Of course, the examination is done based on medical history and monitors the clinical course. In some cases, the disease can have an almost asymptomatic course. Tragically, sudden death can also be the first sign of the disease.
Angiopulmography is one of the basic examination methods, i.e. the insertion of a catheter into a vessel after pushing a contrast agent into the blood vessel. The xamination will show signs of blood vessel congestion, size, shape and number of emboli. Screening techniques, such as CT, CT angiography, and spiral CT scan, perfusion scintigraphy, ventilatory perfusion scan, or chest X-ray may also be used.
An ECG is also performed during the examination. The ECG shows signs of right heart congestion, tachycardia. However, up to 18% of patients with pulmonary embolism have a normal ECG. An ECG is also important to rule out a heart attack.
Echocardiography, sonography, or more specifically, duplex ultrasound of the veins of the lower limbs, are added to the screening. Blood samples will be taken to be tested in a laboratory, where blood gases and other basic blood tests are evaluated. The diagnosis aims to rule out other diseases, such as heart attack, asthma, pneumothorax, bronchopneumonia, chronic obstructive pulmonary disease (COPD).
Course
Pulmonary embolism can run its course in various ways. It depends on the size of the embolus and the extent of vascular occlusion. The course can be mild or typical. Tehre are also asymptomatic forms.
However, massive pulmonary embolism runs a severe course presenting with hemodynamic impairment and cardiogenic shock.
Some data:
In Europe, the incidence is approximately 0.5-1/100,000.
Untreated thromboembolic disease has a high risk of recurrence.
Early anticoagulant treatment reduces the risk of death from this disease by up to 75%.
If left untreated, the condition can end in death. The sufferer may faint or experience cognitive dysfunctions. The most serious symptom is sudden death as the first sign of acute massive pulmonary embolism in a healthy person.
TIP: Learn more about the symptoms of cognitive dysfunctions.
Long-term manifestations include chronic thromboembolic pulmonary hypertension, i.e. cor pulmonale, dilatation, an enlargement of the right heart. Repeated pulmonary embolism is a serious condition. It runs a more severe course in people who have been treated for other heart or lung diseases for a long time.
How it is treated: Pulmonary embolism
Origin and course of pulmonary embolism
Pulmonary embolism is treated by
Pulmonary embolism is examined by
Other names
Interesting resources










