- STANĚK, Vladimír. Cardiology in practice. 2nd updated and extended edition. Axonite s.r.o., publishing house of medical literature, 2020. Asclepius (Axonite CZ). ISBN 978-80-88046-21-9
- solen.cz - Suppurative pericarditis. Solen. Radomír Šímek et al.
- kardiologickarevue.cz - Pericarditis. Cardiodiagnostická revue - Internal medicine online.
- healthline.com - All about pericarditis. Healthline. Marjorie Hecht.
Pericarditis: inflammation of the heart lining. What are its causes and symptoms?
Pericarditis refers to an inflammatory process of the outer lining of the heart (pericardium). It has different etiologies. What is the cause of pericarditis, the first symptoms and treatment options?
Most common symptoms
- Shoulder Blade Pain
- Malaise
- Chest pain
- Muscle Pain
- Spirituality
- Increased body temperature
- Nausea
- Head spinning
- Fever
- Indigestion
- Swelling of the limbs
- The Island
- Hiccups
- Dry cough
- Muscle weakness
- Fatigue
- Anxiety
- Water in the abdomen
Characteristics
Pericarditis is an inflammatory disease of the pericardium (outer lining) of the heart. In many cases, there is a gradual improvement in health without consequences. However, serious complications can occur.
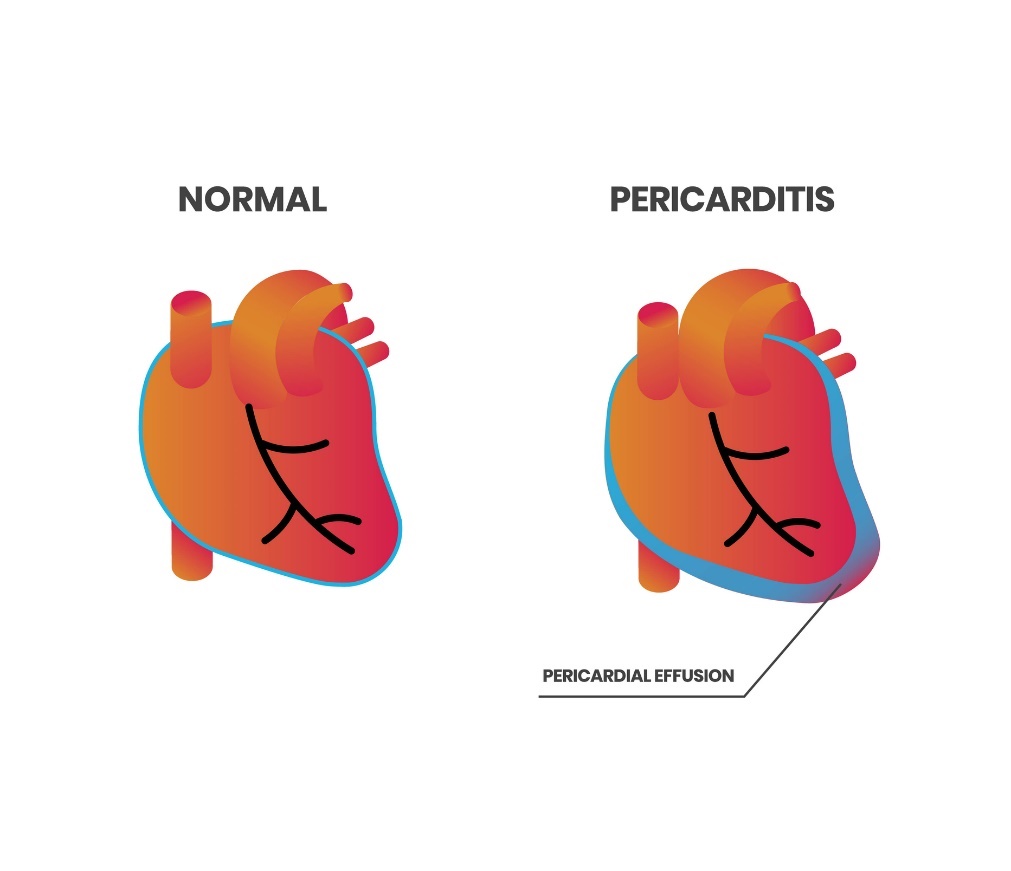
In particular, the risk is the development of cardiac tamponade and pericardial effusion - the accumulation of fluid under the pericardium. What is the etiology of pericarditis, symptoms and treatment options? The answers to these questions and much more can be found in the article.
The heart envelope in a nutshell
The pericardium is a solid protective sac (membrane) surrounding the heart. It consists of 2 sheets, namely, an outer fibrous and an inner serous layer. Under physiological circumstances, there is 20-30 ml of fluid in the pericardial cavity between the two layers.
Below the pericardium is the myocardium (heart muscle) and the inner fibrous layer is the endocardium.
Functions of the pericardium:
- Regulation (restriction) of the movement of the heart
- Protective function against infection of the heart
- Reducing friction of the heart against surrounding tissue
Pericarditis
An inflammatory disease of the heart lining of various etiologies. The characteristic symptom is chest pain on the left side. In some cases it resembles a myocardial infarction. There may also be shooting pain into the left shoulder.
According to the duration of the onset of the inflammatory process, pericarditis is divided into acute and chronic.
Pericarditis is a disease of the pericardium of the heart, in which the pericardial tissue is swollen and inflamed. An inflammatory lesion on an infectious or non-infectious basis is found directly in the pericardium.
This inflammatory process interferes with the physiological function of the heart.
Pericardial effusion is a condition caused by the accumulation of a large amount of fluid between the pericardium and the heart itself. Under physiological circumstances, there is a small amount of fluid in the pericardium which allows the heart to move smoothly within the pericardium.
Cardiac tamponade represents increased pressure on the heart due to excessive fluid or blood formation in the pericardium. The consequence is a reduction in cardiac output and insufficient blood supply to the whole body.
The most serious consequence of the presence of excessive fluid in the pericardium is hemodynamic collapse due to oppression of the cardiac cavities (inability to fill them).
The rapidly forming fluid in acute pericarditis can compress the heart to such an extent that it makes it impossible to fill the right ventricle with blood.
Causes
According to the etiology of its occurrence, pericarditis is divided into infectious and non-infectious types. Infectious cause is more common.
These are mainly viral and bacterial infections, fungi, or parasites.
Viral infections include mainly Coxsackie, Ebstein-Barr virus, echoviruses, enteroviruses, parvoviruses, herpesviruses or HIV. Bacterial infections include Spathyloccocus, Coxiella burnetti or tuberculosis bacteria. Mycotic infections include mainly Hipoplasma and Candida.
Non-infectious pericarditis may arise as a result of autoimmune, metabolic or tumour disease in the vicinity. Systemic lupus, sarcoidosis, rheumatoid arthritis, vasculitis, hypothyroidism or mechanical damage to the pericardium itself.
Dessler's syndrome (pericarditis after myocardial infarction) and postpericardiotomy syndrome in patients after cardiovascular (heart) surgery are also possible.
In clinical practice, the term idiopathic pericarditis is used to refer primarily to acute pericarditis in which the exact aetiology has not been established.
Symptoms
The manifestations of the disease also depend on how quickly pericarditis in the body arose. Acute pericarditis is manifested primarily by a sharp stabbing pain behind the sternum on the left side. It can radiate towards the left shoulder, neck and jaw.
If you develop the above acute symptoms, you should call the emergency services immediately. Especially if the pain is accompanied by vegetative symptoms - sweating, weakness or dizziness.
However, chest pain in pericarditis can also be dull and pressing.
Pericarditis may be accompanied by breathing difficulties, palpitations, coughing, increased fatigue, muscle aches and, if the condition is progressive, severe symptoms of heart failure (swelling of the ankles, calves or abdominal wall).
In the case of chronic pericarditis, the clinical signs may not be very pronounced. The condition develops gradually and the pericardium may adapt to the increased fluid volume to some extent.
Possible symptoms of pericarditis:
- Chest pain
- Heart palpitations
- Dry cough
- Shortness of breath
- Impaired breathing
- Swelling of the lower limbs
- Difficulty swallowing and coughing
- Muscle and joint pain
- Increased body temperature
- Excessive fatigue and weakness
Diagnostics
The specific diagnostic procedure will be determined by the examining physician after taking a medical history, performing a basic initial examination and assessing the patient's clinical symptoms.
The basic principle is the collection of a blood sample and its laboratory evaluation, which confirms or refutes the presence of infectious viruses or bacteria in the body. The values of inflammatory markers (CRP, leukocytosis) determining the presence of inflammation in the patient's body are also detected.
The basic diagnosis of pericarditis includes an ECG (electrocardiography). The electrical activity of the heart is measured. The result is an ECG curve determining the exact waves, oscillations and intervals of the patient's individual heartbeats.
According to the ECG diagnosis, it is possible to detect heart rhythm disorders, the cause of which may be pericarditis.
From physical imaging methods, X-ray examination is used. From the chest image, information can be obtained about the shape and size of the cardiac shadow and the presence of excess fluid (pleural or pericardial effusion) can be determined.
An enlarged spherical cardiac shadow may be a sign of excessive pericardial effusion.
Currently, MRI or CT is preferred. They have higher sensitivity in the early stages of the disease.
MRI (magnetic resonance imaging) and CT (computed tomography) are mainly used to obtain a detailed image of the pericardium. They have the best sensitivity just for showing thickened and calcified pericardium.
Ultrasound echocardiography is useful for detailed imaging of the internal structures of the heart. It describes the size, condition, structure of the heart muscle and valves.
The examination is mainly performed to detect fluid accumulation around the heart. Echocardiography will show the systolic function and any narrowing of the heart chambers.
Cardiac catheterization is used to simultaneously measure the pressures in the heart chambers. A special tube (catheter) is inserted into the venous system. A catheter is inserted directly into the patient's heart.
If a large effusion is present, pericardial fluid analysis (pericardiocentesis) is performed. The fluid is sent for biochemical, microbiological and pathological laboratory analysis.
Pericardiocentesis is also a therapeutic procedure to drain excessive amounts of pericardial fluid.
Forecast
A good prognosis depends on early diagnosis, identification of the cause and expert treatment.
The prognosis of patients with pericarditis is influenced by the intensity of the inflammation and the treatment chosen. Viral pericarditis is in most cases cured without sequelae. The prognosis of pericarditis caused by cardiac damage depends on its severity.
However, any cause of acute pericarditis may persist and lead to subsequent chronic pericarditis.
Diseases that often lead to chronic pericarditis include tuberculosis, radiotherapy and conditions following heart surgery. Thickening, scarring and calcification of the pericardium subsequently restrict the filling of the heart. This results in so-called constrictive pericarditis.
Prevention of pericarditis
Prevention of pericarditis is limited, but certain principles and factors can minimize the risk of its occurrence.
Elimination of the risk of infection, careful hygiene measures and avoiding contact with infectious persons are essential. Vaccination against certain viruses such as influenza or a concomitant vaccine against covid 19 disease is recommended (especially for immunocompromised persons).
If another medical diagnosis is present, professional treatment is required. This will avoid associated medical complications.
An important factor in the prevention of severe pericarditis is early diagnosis. It is necessary to seek medical attention immediately at the first symptoms.
A strong immune system is an essential prerequisite for an easier course of the disease. Regular physical activity, elimination of stress, a balanced, wholesome diet and regular intake of necessary vitamins and minerals are advisable.
How it is treated: Pericarditis
Treatment of pericarditis: medication, puncture, surgery
Show morePericarditis is treated by
Other names
Interesting resources
Related










