- "What Are the Signs and Symptoms of Coronary Heart Disease?". www.nhlbi.nih.gov.
- "Heart Attack Symptoms in Women". American Heart Association.
- "What Is a Heart Attack?". www.nhlbi.nih.gov.
- "Heart Attack or Sudden Cardiac Arrest: How Are They Different?".
- Mehta PK, Wei J, Wenger NK (February 2015). "Ischemic heart disease in women: a focus on risk factors". Trends in Cardiovascular Medicine. 25 (2): 140–51.
- Mendis S, Puska P, Norrving B (2011). Global atlas on cardiovascular disease prevention and control (PDF) (1st ed.). Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3–18.
- "How Is a Heart Attack Diagnosed?". www.nhlbi.nih.gov.
- Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. (October 2012). "ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation". European Heart Journal. 33 (20): 2569–619.
- O'Connor RE, Brady W, Brooks SC, Diercks D, Egan J, Ghaemmaghami C, et al. (November 2010). "Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S787–817.
- Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (GBD 2015 Disease Injury Incidence Prevalence Collaborators) (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602.
- Coventry LL, Finn J, Bremner AP (2011). "Sex differences in symptom presentation in acute myocardial infarction: a systematic review and meta-analysis". Heart & Lung. 40 (6): 477–91.
- Valensi P, Lorgis L, Cottin Y (March 2011). "Prevalence, incidence, predictive factors and prognosis of silent myocardial infarction: a review of the literature". Archives of Cardiovascular Diseases. 104 (3): 178–88.
- mayoclinic.org - Heart attack
- health.harvard.edu - Heart Attack (Myocardial Infarction)
Myocardial infarction: Why does it occur, what are the manifestations of an acute heart attack?

Myocardial infarction or even heart muscle infarction is an acute form of ischemic heart disease. Ischemia, or bloodlessness, is caused by a blockage in the coronary artery that leads blood to the heart muscle cells. The main cause is a sudden closure or long-term narrowing of the blood vessel.
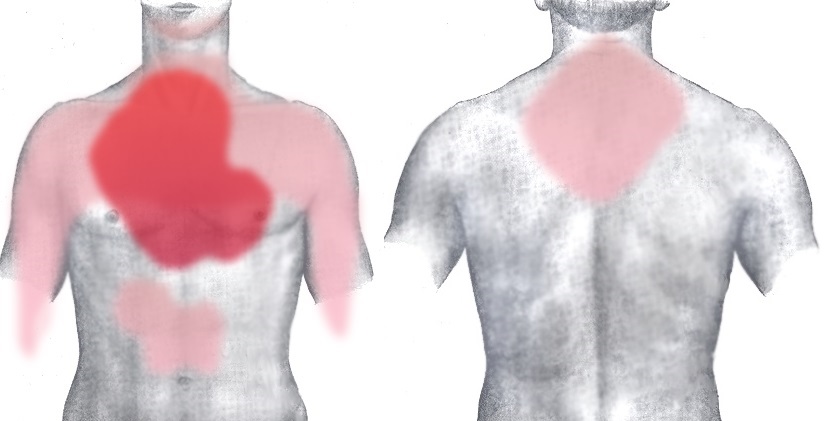
Most common symptoms
- Shoulder Blade Pain
- Malaise
- Chest pain
- Shooting pain in fingers and toes
- Pain that Radiates into the Shoulder
- Spirituality
- Blue leather
- Sweating
- Nausea
- Low blood pressure
- Lung Island
- Disorders of consciousness
- Anxiety
- Slowed heartbeat
- Muscle weakness
- Pressure on the chest
- Fatigue
- Vomiting
- High blood pressure
- Confusion
- Accelerated heart rate
Characteristics
If ischemia of the heart muscle cells occurs, it is a heart attack.
Myocardial infarction is an acute bloodless cell attack, therefore it is also referred to as acute myocardial infarction (AMI). If the cells of the heart muscle are without blood circulation for a long time, nourishment and oxygenation, necrosis occurs, ie their death. This necrosis occurs in an area supplied by a clogged cardiovascular system.
Heart attack is one of the most common causes of death worldwide.
Cardiac vessels are those that serve to supply blood to the heart itself. They are also referred to as coronary or coronary vessels. During a long-term pathological process, known ischemic heart disease occurs, also referred to as coronary heart disease. It is based on atherosclerosis.
Atherosclerosis is a long-term degenerative disease in which the hardening of the vascular wall occurs by storing fats and leukocytes. The vessel wall solidifies over time, its lumen narrows (inner diameter). Atherosclerotic plaques are formed, which are deposited in the artery wall. The result is impaired flow and blood flow through the artery.
If this atherosclerotic plaque ruptures, the vessel wall is disrupted. Subsequently, platelets are applied, so-called intracoronary thrombosis occurs. This thrombosis can partially or completely restrict blood flow to the heart muscle.
TIP: information in the article on atherosclerosis at the Medical Center.
Atherosclerotic vessels are the cause of impaired blood flow to the heart, especially if the heart muscle has a higher demand for blood supply. An example is physical activity, but also mental stress. Then the heart rate, ie the heart rate, increases.
If the heart muscle is insufficiently congested, chest pain develops, also known as angina pectoris (AP). People often describe this pain as pressure on their chest or even as if someone was sitting on their chest, or as if they had a stone on their chest.
Read also: Chest pain and chest t i ghtness also occur for other causes.
In angina pectoris, ie transient chest pain, the symptoms usually subside within 15 minutes. . If the cause was exertion, then when the load and rest were interrupted. The burden can be physical or mental. For example, running, fast walking, in case of severe damage to a blood vessel, and walking for a few meters.
An example of a psychological burden is agitation or an argument.
However, if the chest pain lasts longer than 15 minutes, it is necessary to think about a heart attack. The pain does not go away at rest or after the administration of nitroglycerin (NTG). When you do not bleed, necrosis begins to develop, which means that the muscle cells die.
Ischemic damage occurs in as little as 20 minutes. At this stage, it is still reversible and can be reversed. Of course, the longer the heart muscle cells (cardiomyocytes) are bloodless, the worse the damage. Already after 2 hours occurs myocardial cells and necrosis, which is irreversible (irreversible).
Naturally, how quickly irreversible cell damage occurs is individual. The timestamp can affect, for example, the condition of the heart or collateral coronary supply. This is the supply of the area of ischemia from another coronary artery.
If the ischemic reserve is depleted, muscle necrosis can occur after as little as 20 minutes. However, after 4-9 hours there is massive damage to the heart muscle, the so-called transmural heart attack. It affects the entire thickness of the heart wall.
You ask:
Is there such a thing as a transient or mild heart attack?
There is no such thing as a heart attack.
The man was simply fortunate to have survived without serious consequences or death without diagnosis and adequate treatment. People tend to call it a mild heart attack.
However, it is not so easy even with such a seemingly mild course. Dead heart muscle cells are there and nothing can cure them. And dead muscle is not fulfilling its function.
The damaged muscle may require restrictions.
We continue ...
The organism cannot regenerate damaged heart cells, it does not create new ones. The dead area heals with a scar. The scar is down. Consequently, reduced heart function develops. There is also a risk of rupture of this scar and bleeding into the pericardium, the so-called heart tamponade - pericardium.
Interesting information:
Due to its size, the heart muscle has the highest demand and oxygen consumption among other organs in the body.
The heart works continuously, without stopping or pausing for 24 hours.
At rest, the blood flow through the heart vessels is approximately 250 ml.
During exercise, the blood flow can increase up to 5 times.
What is acute coronary syndrome?
Acute coronary syndrome, abbreviated ACS, is a collective term for unstable angina, acute myocardial infarction, and sudden death caused by coronary artery occlusion. ACS is divided based on changes in the ECG. An ECG is an examination of the electrical activity of a cardiac conduction system.
An acute coronary syndrome is divided into:
- STAKS, or STEMI, means ST elevation on the ECG in myocardial infarction
- NSTAKS, ie NON-STEMI, NSTEMI, and this designation may include two subunits:
- unstable angina pectoris (NAP)
- NSTEMI, ie myocardial infarction without ST elevation on the ECG
If we want to go into detail, the ACS is further divided according to ECG changes into STEMI and NON-STEMI (NSTEMI).
Marginally, this means whether ST-segment elevation is present on the ECG in the case of STEMI, and thus coronary artery occlusion.
Or ...
ST-elevation on ECG is not present = NON - STEMI when at least partial perfusion of the heart muscle is maintained.
+
A patient with STEMI is indicated for primary reperfusion therapy (angioplasty) in a cardio center (PKI center). And preferably within 12 hours of the onset of difficulties.
Further management of the patient by the emergency medical service is:
Ideal transport of the patient from the detection of ST-elevation on the ECG,
ie diagnosis of STEMI and
time of arrival to the PKI center =
90 minutes - more precisely 90 + 30 minutes (interval in PKI)
= 120 minutes from detection of STEMI to admission in the PKI center.
AKS includes three subunits, and thus:
- Unstable angina pectoris (NAP) is ischemia (bloodlessness) of the heart muscle
- it can arise in peace, without effort or another factor
- worsened or altered AP in the case of existing stable angina pectoris
- myocardial infarction is the death of the heart muscle, which occurs in as little as 15-20 minutes of non-blood flow to the heart muscle
- the final death of cardiac muscle cells occurs within 9-12 hours of occlusion
- Sudden death is defined as death that occurred within one hour of the onset of the disorder
- up to 70% of them have a cause in coronary heart disease
- maybe the first manifestation of the disease.
We may also encounter another sign of a heart attack. And as transmural, nontransmural, or Q-wave and non-Q-wave myocardial. However, the division into STEMI and NSTEMI is of great importance in subsequent treatment management.
In the case of myocardial infarction, we may also encounter a division according to the affected area of the heart. The location is determined by the vessel's involvement. The main ones are the artery coronaria dextra (ACD) and the arteria coronaria sinistra (ACS), ie the right and left coronary arteries. These two main arteries extend directly from the aorta. They further branch into smaller coronary arteries.
Some coronary vessels such as:
- dextra coronary artery - ACD
- sinus coronary artery - ACS
- anterior interventricular frame - RIA
- posterior interventricular frame - RIP
- ramus circumflexus - RCx
- ramus marginalis sinister - RMS
- ramus coni arteriosi - Rco
- ramus nodi sinuatrialis - Rns
- dexter posterolateral ramus - RPLD
- ramus diagonalis (lateralis) - RD
The table shows the distribution of IM by area.
| IM name | Description |
| Front wall | or also anteroseptic when affecting the RIA vessel basin |
| Anterolateral | IM affects the RIA basin |
| Lateral | thus the lateral artery may be affected: RCx, RD, RMS, RPLD |
| Bottom | also referred to as diaphragmatic vessels: ACD and RCx |
| The back wall | hits the RCx vessel |
| Right ventricle | affected coronary artery ACD |
Causes
Myocardial bleeding is due in most cases to atherosclerosis.
The atherosclerotic plaque ruptures in the vessel wall (rupture of the atherosclerotic plaque). Platelets attach to the damaged vascular wall, and intracoronary thrombosis, or thrombus in the vascular lumen, occurs.
Read also: Article Ischemic heart disease at Nursing.
This thrombus causes the vessel to narrow (its inner diameter). The result is reduced blood flow to the rest of the artery.
With a greater extent of thrombosis, coronary artery occlusion occurs and blood flow stops completely. This leads to ischemia, ie bloodlessness after 15 - 20 minutes.
Irreversible death, ie necrosis of bloodless heart cells, occurs within approximately 2 hours.
The reasons for the restriction to complete cessation of blood flow through the coronary artery are:
- atherosclerosis with thrombosis
- vascular spasm - contraction of blood vessels, even as a result of cocaine ingestion
- arteritis ( inflammation of the blood vessel )
- embolization
- thrombosis without atherosclerosis
Unstable angina or NSTEMI occurs when the blood flow through the vessel is partially restricted (non-occlusive thrombus). This form may not have clinical manifestations, until the time of increased cardiac muscle demand.
If the vessel is completely closed by a thrombus (occlusive thrombus), STEMI or sudden cardiac death results.
STEMI, or acute myocardial infarction, or AIM, has its typical symptoms.
However, in some cases, it may also be atypical or Nemo- asymptomatic.
In many cases, sudden cardiac death is the first sign of the disease in a previously healthy person.
We know some of the risk factors that lead to AIM, their table shows
|
|
Interesting information about:
Blood pressure values and
What are the typical symptoms of high blood pressure?
Symptoms
I'm sure you've heard that a person has overcome IM and didn't even know it.
Sudden cardiac death also falls under the term ACS. Heart death is a serious complication of a heart attack. And it is very worrying that in some cases it is the first sign of the disease in a hitherto healthy person.
Sudden cardiac death occurs immediately after the coronary artery is closed or within an hour of the onset of the problem.
Symptoms of myocardial infarction in the wand
|
|
The variability of the symptoms depends on the location, the extent of the involvement of the heart muscle, and thus on the area of the closed cardiac bloodstream.
The alarming figure is that up to 45% of people with MI die within 4 hours of the onset of the problem.
Half of the deaths are outside the medical facility. In particular, young people are at risk for familial occurrence and genetic predisposition, blood lipid disorders, diabetes, and cocaine abuse.
The prognosis and survival of an affected person depend equally on the extent of MI, but also on the early recognition of difficulties and early professional treatment. Neither home treatment nor alternative treatment helps.
Complications of myocardial infarction
The heart muscle ischemia itself seriously endangers human health and life. However, various complications can occur with a heart attack. Left heart failure results in left heart failure to cardiogenic shock. This leads to shortness of breath and pulmonary edema.
Articles in the Diseases section:
Heart Failure
Shock - General Information
Cardiogenic S hock
Pulmonary edema is a swelling of the lungs that results from failure of left ventricular function. Blood accumulates in front of the left ventricle. Fluid from the blood vessels passes into the lungs. This is typically manifested by shortness of breath and respiratory crusts present, up to audible bubbling when breathing at a distance.
For more information on pulmonary edema, see the article on Health.
Cardiac muscle ischemia results in various biochemical changes and impaired cell metabolism. This can also result in cardiac arrhythmias. Ventricular fibrillation is severe. There is also a risk of systemic embolization, for example into the brain when a sudden stroke or kidney occurs.
Other risks include aneurysms, ventricular septal defects, valve defects, as well as rupture of the heart wall and subsequent pericardial tamponade.
Diagnostics
Of course, the timing of the duration of the difficulties is important.
Typical symptoms lead to a diagnosis. There are other associated symptoms of a heart muscle infarction that may help to suspect that it is a heart attack. Of course, whether the cause of the problem is a heart attack or other illness will be assessed by a healthcare professional.
Therefore, it is important to call 155 if symptoms occur. Because, chest pain can hide various diagnoses, such as:
- aortic dissection
- pulmonary embolism
- pleurisy
- GERD or oesophagitis
- gastric and duodenal ulcers
- panic attack and anxiety
- difficulty with the spine
Healthcare professionals also perform examinations such as ECGs. An ECG is the basic examination method used to diagnose AIM. This examination assesses whether it is STEMI or NSTEMI. This is important in the subsequent treatment strategy. A person with STEMI is indicated for primary reperfusion therapy in the cardio center, ie in the PKI center.
ECG examination is available in the ambulances of the emergency medical service (EMS), which is a component of pre-hospital and emergency health care. In primary care with a general practitioner (not all general practitioners have an ECG). But also for a specialist in the outpatient clinic of an internist or cardiologist.
If it is not clear whether it is an IM, blood sampling may be supplemented when assessing blood baseline blood parameters, but especially troponin. In necrosis, troponin is released from the necrotizing heart muscle cells.
Pre-hospital management of ACS
Before a person with acute coronary syndrome gets to the hospital, it is necessary to ensure appropriate prehospital management. Of course, it depends on the situation. A person can be at home, on the street or in a GP's office, or in a specialist's office.
However, it is important to:
- quick diagnosis
- early treatment
- directing the patient to the PKI center or administrative hospital
The table provides information on AKS
| Acute coronary syndrome | |||
| TYPE | STEMI | NSTEMI | Unstable AP |
| History | chest pain | chest pain | chest pain |
| Call 155 | |||
| ECG | ST-elevation fresh block LBBB or bifascicular block | ST depression changes T wave | ST depression changes T wave |
| Biochemistry | positive troponin | positive troponin | negative troponin |
| Treatment |
early treatment of ASA, namely aspirin Tikagrelol or prasugrel, clopidogrel or heparin give anything im | do not give them anything | do not give them anything |
| Routing |
primary reperfusion treatment cardiocenter, PKI center time up to 120 minutes but optimally up to 90 minutes from ECG diagnostics STEMI | hospital | hospital |
|
Routing patients depends mainly on diagnosing STEMI, but also on the timestamp If a long time to ECG diagnosis after coming to Cardio, chooses the other medical management, and fibrinolysis in EMS or hospital | |||
| KPR
in case of sudden cessation of blood circulation immediate chest compression use of AED - automatic external defibrillator the a most common cause of cessation of circulatory disorders is a heart rhythm, namely ventricular tachycardia and fibrillation | |||
| WARNING
very important in the early recognition of the symptoms of ACS time loss can cause delays inadequate treatment of IM health complications to sudden death | |||
Angioplasty, a demonstration of PKI
The table shows the important time intervals for ACS
| Title | Ideal time period | Description |
| Development of difficulties up to ECG | up to 10 minutes | is the ideal time after diagnosis of AIM beware of neglect of the problem on the part of the affected person or doctor deteriorates the treatment strategy increases the risk of complications |
| ECG - thrombolysis (needle) | up to 30 minutes | if the time range of the PKI center is not recommended, the time delay of diagnostics |
| ECG - PKI | up to 120 minutes optimally up to 90 minutes | intervention in the cardio center is also referred to as ECG - balloon interval from STEMI diagnosis on the ECG to arrival at the cardio center |
| ECG - PKI with extensive anterior IM | up to 90 minutes optimally up to 60 minutes | |
| ECG - coronary angiography after thrombolysis | 3 - 24 hours | |
| The total ischemic time is the time from the onset of symptoms to the introduction of the balloon into the affected vessel and its passage | ||
Course
Such as the location and extent of vascular bed involvement , and thus the area of ischemia, the current state of the heart , but also the presence of collateral blood supply .
Myocardial infarction can have a typical course .
However, in some cases it is atypical , even when it is asymptomatic , it is hidden .
The typical course of h is characterized by pain behind the sternum or chest. Pain may be non-specific when referred to as chest discomfort. But it can be pressurized, hot, or animal. One describes the feeling of someone sitting on his chest or having a stone on his chest.
The pain is in one place, but often radiates to the shoulders, left upper limb, neck or sled, or between the shoulder blades. Cardiac ischemia lasts longer than 15 - 20 minutes, so the pain persists. It does not respond to nitrates or common analgesics.
Associated with difficulty breathing, paleness, sweating. One can feel fear of death and anxiety. Of course, if these symptoms occur together or in different combinations, there is no need to wait for the difficulties to go away. Immediate help is needed.
A heart rhythm disorder, palpitations may be present during a heart attack. But also other neurological problems or worsening of the mental state, such as confusion. Then there is a suspicion of embolization into the vascular bed of the brain, ie a stroke.
One may lose consciousness for a short time, fall away, but then take over. Impaired consciousness can also be caused by circulatory arrest. This is often the result of ventricular fibrillation or tachycardia. In this case, it is important to recognize and initiate CPR, that is, chest compressions.
If it is within range of the AED, the automatic external defibrillator must be used.

Heart attack is one of the most common causes of sudden death. This is despite a good network of pre-hospital care and the availability of a cardio center or PKI center. Sudden cardiac death occurs within or within 1 hour of the onset of the problem. It is often the first symptom in a healthy person.
TIP: For more information on stopping blood circulation, see the article on arrhythmias.
Video about CPR:
First aid for myocardial infarction
Myocardial infarction is an acute condition and endangers a person's health and life. Therefore, it is necessary to recognize typical symptoms in time and react immediately . If you notice these symptoms, you need to act quickly.
Early detection and rapid treatment are important for the future condition of the heart and its function.
First aid:
- Sit the affected person comfortably, lean him against something, for example on the floor against the wall
- be with him
- calm him down
- it is forbidden to eat or drink
- do not smoke or drink alcohol
- emergency medical service should be called 155 immediately
- it is ideal to give him a medicine containing acetylsalicylic acid (ASA), such as Anopyrin, Aspirin, Acylpyrin at a dose of 400 mg
- beware of allergies
- if the victim has ischemic heart disease or has already had a heart attack
- should take ASA immediately
- if prescribed nitroglycerin (NTG) or other nitrates (spray)
- be careful when administering NTG, the blood pressure must be higher than 100, otherwise, there is a risk of collapse and loss of consciousness
- nitrates should not be used if a person has taken sildenafil - Viagra and similar products for 48 hours
- the condition of the victim must be monitored until the arrival of the assistance
- keep in mind that the risk of complications may be higher, especially during periods of extreme heat
- when CPR circulation is stopped, call back 155 - the operator will guide you to the correct procedure
- if an AED (Automated External Defibrillator) is available - use it
- CPR until the arrival of assistance

Threatening statistics and possible prevention
The statistics of this heart disease are quite serious and terribly surprising. Every year, more than 17 million people die of myocardial infarction in the world, and in our country, it is several thousand. In practice, this means that every minute someone in Europe dies of myocardial infarction.
And that is why the disease should not be underestimated. The wrong lifestyle and bad lifestyle are also to blame for the high numbers. And so prevention is more important than ever. Which factors are at risk for heart attacks and which are preventive?
The following table provides a quick overview of the answers:
| Factor | Influence on the incidence of infarction |
| High blood pressure and high cholesterol | risk impact |
| Smoking and excessive alcohol consumption | risk impact |
| Diabetes, overweight, and obesity | risk impact |
| Family history | risk impact |
| Fruits and vegetables every day | preventive effect |
| Plenty of exercises every day | preventive effect |
| Maintaining cholesterol and blood pressure | positive impact |
| Sufficient drinking regime | positive impact |
| Avoiding heavy and greasy foods | positive impact |
| Preventive inspections | preventive effect |
| Treatment of risk factors | preventive effect |
+ Wondering how to live after a heart attack and what limitations may await you ?You can find the answers to these questions and a lot of other interesting information in the article: What is life like after a heart attack? Does it have limitations, will it cause incapacity for work?
How it is treated: Myocardial infarction
What is the treatment for heart muscle infarction? Medical emergency, medications and intervention
Show moreMyocardial infarction is treated by
Myocardial infarction is examined by
Interesting resources










