Hydrocele of the testicle is also popularly called water hernia.
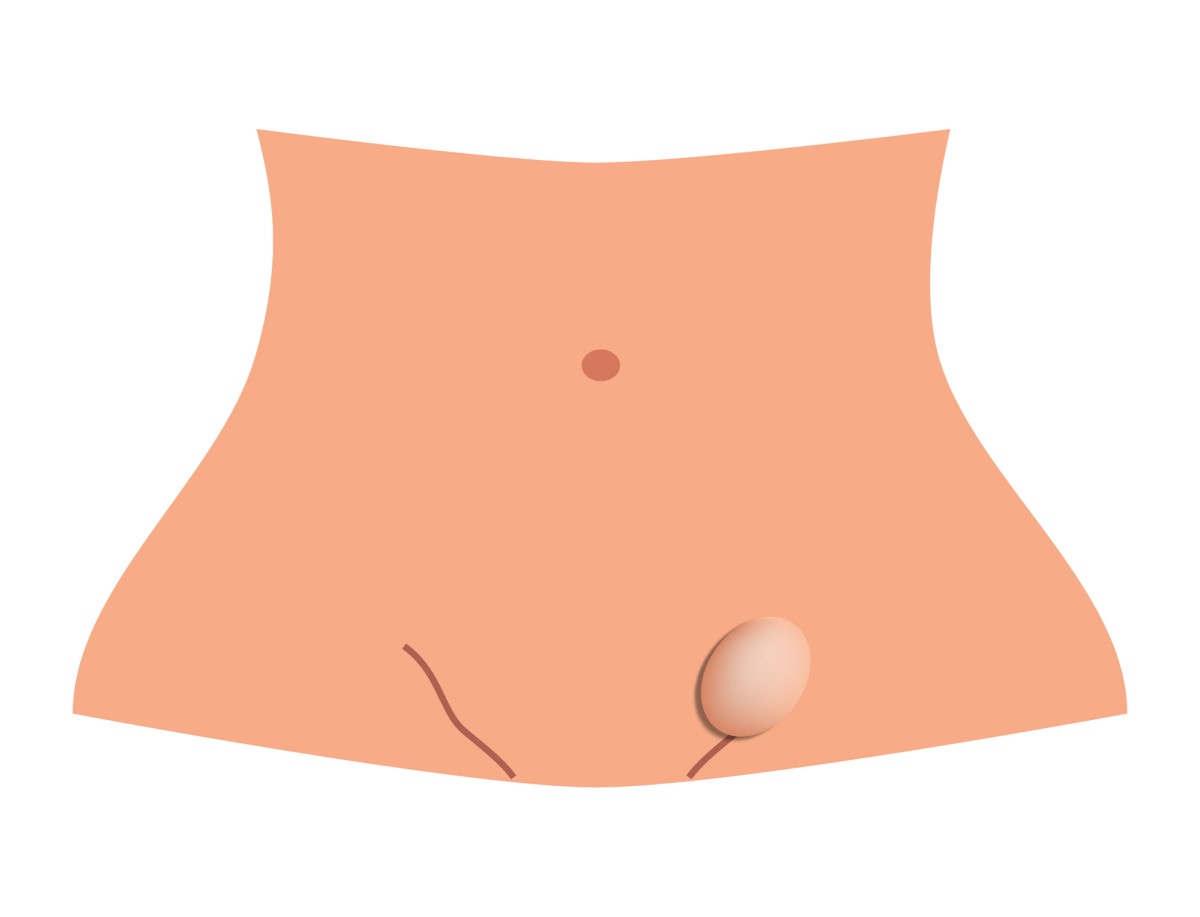
This is a buildup of serous fluid in the scrotum, causing it to swell and enlarge.
Normally, the between the lining of the testicle only a small amount of fluid.
If blood accumulates in the testicles, this condition is called hematochezia.
Hydrocele often occurs in children and young boys. In adulthood, it is usually caused by an accident or infection around the genitals.
In hydrocele, varying amounts of fluid may accumulate in the lining of the testicles and its resorption may be reduced. This leads to subsequent fluid accumulation and testicular enlargement.
Hydrocele does not affect male fertility and poses no danger to the testicles.
Male genital organs
The testis is an egg-shaped paired gland located in the scrotum and covered by a whitish membrane.
The function of the testes is to produce sperm.
For proper function and because of the need to maintain a lower temperature, the testicles are stored outside the body in the scrotum. This achieves a lower temperature than in the abdominal cavity.
The epididymis is a long formation located at the back of the testicle, wider at the top, overlapping the testicle.
The fallopian tube (ductus deferens) passes from the epididymis upward, through the inguinal canal, and connects to the urethra.
Blood vessels pass through the scrotum and inguinal canal along with the seminiferous ducts. The blood vessels of the testes and the vas deferens are surrounded by a muscular sheath that forms the so-called seminal cord.
The seminal vesicles (vesiculae seminales) are small sac-like organs located on the sides of the bladder. They produce a sticky mass that inhibits the movement of sperm.
The prostate gland (prostate) is located below the bladder. It produces a thin, cloudy secretion that mixes with semen and mucus from the epididymis to form ejaculate.
The scrotum is the skin sac in which the testicles are located. The scrotum is divided into two halves by a septum. The skin of the scrotum is soft and has hairs on its surface.
The terminal part of the male sex organ is the glans penis, inside which is the urethra.
The course of descent of the testicles of the fetus
Already during intrauterine development of the fetus, the testicles, which separate the abdominal cavity from the scrotum, descend.
Descending downwards, the testes pass through the inguinal canal until they reach the scrotum. Along with the seminiferous tubules, the processus vaginalis, the connection between the peritoneum and the scrotum, also descends.
At birth, the testicles are already descended and the processus vaginalis is closed. Two sheets remain on the front of the testicles. If it fails to close, fluid is deposited in this space and a hydrocele forms.
Read also the article.
Hydrocele in children
The processus vaginalis allows communication between the scrotum and the peritoneum. It is a protrusion of the peritoneum protruding into the inguinal canal already during the development of the male fetus in the uterus before the descent of the testes. It disappears after the descent of the testes.
If there has been no separation of the abdominal cavity from the scrotum, the fluid in the abdominal cavity enters the inguinal canal and descends into the testes.
In newborns, the occurrence of hydrocele is not uncommon, but in most cases, this deficiency is corrected by 1 year of age. If it continues to persist, it must be corrected surgically.
Distribution of hydrocele
Hydrocele is divided into primary and secondary.
Primary hydrocele
Primary hydrocele is also called as communicating or congenital hydrocele. It arises after incomplete closure of the amniotic sacs during fetal development with a persistent opening through which fluid from the abdominal cavity flows into the scrotum.
The hydrocele communicates. That is, it's in contact with the fluid in the abdominal cavity.
This type of hydrocele is characterised by the size of the scrotum, which changes during the day as fluid moves from the scrotum into the abdominal cavity.
Hydrocele of the spermatic cord occurs after the closure of the sac and leaves fluid in the spermatic cord. In children, it is referred to as processus vaginalis of the spermatic cord. This changes during intrauterine development before birth or after birth during 1-2 years and closes the communication between the abdomen and scrotum.
Primary hydrocele can occur at puberty, even if it has not manifested by then, but also in men in middle and later age.
Hydrocele of the canal of Nuck occurs in women. It is a fluid accumulation at the site of the vaginal entrance and the labia majora. It is manifested by swelling of the labia majora or swelling in the groin.
Secondary hydrocele
Secondary hydrocele is also known as non-communicating, reactive or acquired hydrocele. It is caused by another condition, such as fluid left in the seminal vesicle after the closure of the anus. It can also result from inflammation, infection, trauma, as well as a tumour or testicular torsion.
Non-communicating hydrocele occurs when the inguinal canal is closed but there is excess fluid in the scrotum. It occurs because fluid has remained in the scrotum after the canal is closed and there is no connection to the abdominal cavity through which the fluid can return to the abdomen.
It can also occur in newborns, but also in men at an older age without any cause.
This type of hydrocele is usually small, grows slowly or remains unchanged for years. The exception is filariasis (a tropical infection caused by parasitic worms), where the hydrocele can grow to large proportions.
Fluid accumulation in the testes may also result from an imbalance in the rate of fluid production and reabsorption.
It occurs most commonly in adolescent and adult males.
Reactive hydrocele occurs as a result of inflammation, infection, scrotal trauma, or testicular curl in the scrotum. It is one of the non-communicating hydroceles.
Read: Varicocele: How do scrotal varices manifest?