- "Nonalcoholic Fatty Liver Disease & NASH". National Institute of Diabetes and Digestive and Kidney Diseases. November 2016.
- Singh, S; Osna, NA; Kharbanda, KK (28 September 2017). "Treatment options for alcoholic and non-alcoholic fatty liver disease: A review". World Journal of Gastroenterology. 23 (36): 6549–6570.
- Antunes, C; Azadfard, M; Gupta, M (January 2019). "Fatty Liver".
- Basra, Sarpreet (2011). "Definition, epidemiology and magnitude of alcoholic hepatitis". World Journal of Hepatology. 3 (5): 108–113.
- Iser, D; Ryan, M (July 2013). "Fatty liver disease—a practical guide for GPs". Australian Family Physician. 42 (7): 444–7.
- Chalasani, Naga; Younossi, Zobair; Lavine, Joel E.; Charlton, Michael; Cusi, Kenneth; Rinella, Mary; Harrison, Stephen A.; Brunt, Elizabeth M.; Sanyal, Arun J. (January 2018). "The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases". Hepatology. 67 (1): 328–357.
- Singh, Siddharth; Allen, Alina M.; Wang, Zhen; Prokop, Larry J.; Murad, Mohammad H.; Loomba, Rohit (April 2015). "Fibrosis Progression in Nonalcoholic Fatty Liver vs Nonalcoholic Steatohepatitis: A Systematic Review and Meta-analysis of Paired-Biopsy Studies". Clinical Gastroenterology and Hepatology. 13 (4): 643–654.e9.
- Younossi, Zobair; Anstee, Quentin M.; Marietti, Milena; Hardy, Timothy; Henry, Linda; Eslam, Mohammed; George, Jacob; Bugianesi, Elisabetta (20 September 2017). "Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention". Nature Reviews Gastroenterology & Hepatology. 15 (1): 11–20.
- Qian Y, Fan JG (May 2005). "Obesity, fatty liver and liver cancer". Hepatobiliary & Pancreatic Diseases International. 4 (2): 173–7.
- Bellentani, Stefano (January 2017). "The epidemiology of non-alcoholic fatty liver disease". Liver International. 37: 81–84.
Fatty liver disease: Definition, Causes, Manifestations, Treatment
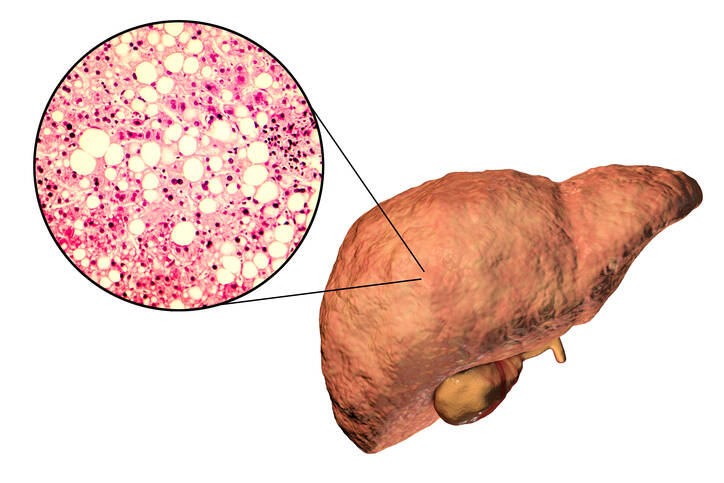
Photo source: Getty images
Most common symptoms
- Malaise
- Right Flank Pain
- Abdominal Pain
- Nausea
- Constipation
- Diarrhoea
- Bleeding
- Flatulence - bloating
- Bloating - flatulence
- Overweight
- The Island
- Disorders of consciousness
- Stool with blood - blood in the stool
- Muscle weakness
- Fatigue
- Water in the abdomen
- Vomiting blood
- Vomiting
- Yellowish skin
- Liver enlargement
Show more symptoms ᐯ
How to treat fatty liver? Medication, diet. No alcohol, protect the liver
Show moreFatty liver disease is treated by
Other names
steatosis, steatosis hepatica, steatosis heparu, fatty liver disease, fatty liver, fatty liver, fatty liver, non-alcoholic fatty liver disease, non-alcoholic fatty liver, NAFL










