- "Diverticular Disease". www.niddk.nih.gov. September 2013. Archived from the original on 13 June 2016. Retrieved 12 June 2016.
- Tursi, A (March 2016). "Diverticulosis today: unfashionable and still under-researched". Therapeutic Advances in Gastroenterology. 9 (2): 213–28. doi:10.1177/1756283x15621228. PMC 4749857. PMID 26929783.
- Pemberton, John H (16 June 2016). "Colonic diverticulosis and diverticular disease: Epidemiology, risk factors, and pathogenesis". UpToDate. Archived from the original on 2017-03-14. Retrieved 13 March 2017.
- Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. Churchill Livingstone. 2014. p. 986. ISBN 9781455748013. Archived from the original on 2016-08-08.
- Young-Fadok, TM (October 2018). "Diverticulitis". New England Journal of Medicine. 379 (17): 1635–42. doi:10.1056/NEJMcp1800468. PMID 30354951. S2CID 239933906.
- Feldman, Mark (2010). Sleisenger & Fordtran's Gastrointestinal and liver disease pathophysiology, diagnosis, management (9th ed.). [S.l.]: MD Consult. p. 2084. ISBN 9781437727678. Archived from the original on 2016-08-08.
- Young-Fadok TM (2018). "Diverticulitis". The New England Journal of Medicine. 379 (17): 1635–1642. doi:10.1056/NEJMcp1800468. PMID 30354951. S2CID 239933906.
- Swanson SM, Strate LL (2018). "Acute Colonic Diverticulitis". Annals of Internal Medicine. 168 (9): ITC65–ITC80. doi:10.7326/AITC201805010. PMC 6430566. PMID 29710265.
- Templeton, AW; Strate, LL (August 2013). "Updates in diverticular disease". Current Gastroenterology Reports. 15 (8): 339. doi:10.1007/s11894-013-0339-z. PMC 3832741. PMID 24010157.
- Böhm, Stephan K. (29 April 2015). "Risk Factors for Diverticulosis, Diverticulitis, Diverticular Perforation, and Bleeding: A Plea for More Subtle History Taking". Viszeralmedizin. 31 (2): 84–94. doi:10.1159/000381867. PMC 4789955. PMID 26989377.
- Ferguson LR, Laing B, Marlow G, Bishop K (January 2016). "The role of vitamin D in reducing gastrointestinal disease risk and assessment of individual dietary intake needs: Focus on genetic and genomic technologies". Mol Nutr Food Res. 60 (1): 119–33. doi:10.1002/mnfr.201500243. PMID 26251177.
- Weisberger, L; Jamieson, B (July 2009). "Clinical inquiries: How can you help prevent a recurrence of diverticulitis?". Journal of Family Practice. 58 (7): 381–2. PMID 19607778.
- Morris, AM; Regenbogen, SE; Hardiman, KM; Hendren, S (Jan 15, 2014). "Sigmoid diverticulitis: a systematic review". JAMA. 311 (3): 287–97. doi:10.1001/jama.2013.282025. PMID 24430321.
- Lee, Kyoung Ho; Lee, Hye Seung; Park, Seong Ho; Bajpai, Vasundhara; Choi, Yoo Shin; Kang, Sung-Bum; Kim, Kil Joong; Kim, Young Hoon (2007). "Appendiceal Diverticulitis". Journal of Computer Assisted Tomography. 31 (5): 763–9. doi:10.1097/RCT.0b013e3180340991. PMID 17895789. S2CID 1027938.
- Onur MR, Akpinar E, Karaosmanoglu AD, Isayev C, Karcaaltincaba M (February 2017). "Diverticulitis: a comprehensive review with usual and unusual complications". Insights into Imaging. 8 (1): 19–27.
Diverticulosis and diverticulitis: What are its causes and symptoms? + Treatment
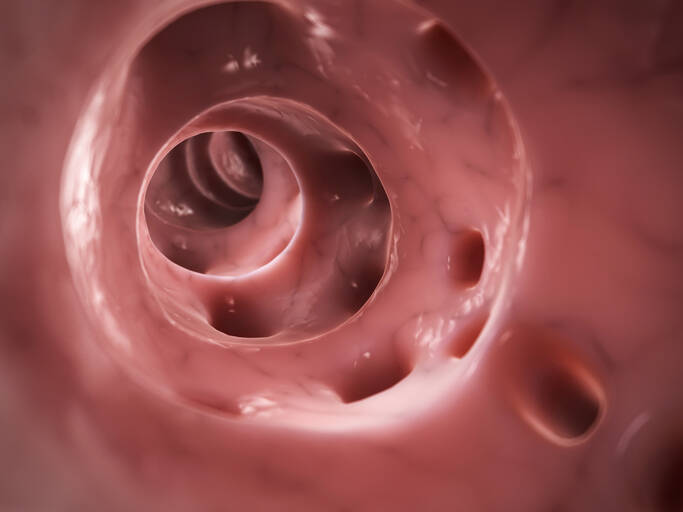
Photo source: Getty images
Most common symptoms
- Malaise
- Abdominal Pain
- Lower Abdominal Pain
- Groin Pain
- Back Pain
- Fever
- Increased body temperature
- Cramps in the abdomen
- Nausea
- Constipation
- Diarrhoea
- Bleeding
- Flatulence - bloating
- Bloating - flatulence
- Indigestion
- Stool with blood - blood in the stool
- Fatigue
- Vomiting
- Stuck winds - stopping the outflow of gases
- Winterreise
- Accelerated heart rate
Show more symptoms ᐯ
Diverticulosis - treatment: medication, diet modification and surgery
Show more









