- solen.sk - PRINCIPLES AND OPTIONS OF SURGICAL TREATMENT OF COLORECTAL CARCINOMA, Karel Kroupa
- cancer.gov - Colon Cancer Treatment (PDQ®)
- emedicine.medscape.com - Colon Cancer
- medlineplus.gov - Colorectal Cancer
- webmd.com - Colorectal Cancer Health Center
- mayoclinic.org - Colon Cancer
Colon cancer: is prevention possible? Yes! What are the symptoms?
Colon cancer (colorectal cancer) is a malignant tumour arising from the inner wall of the colon or rectum.
Most common symptoms
- Malaise
- Abdominal Pain
- Anal pain
- Painful bowel movements
- Cramps in the abdomen
- Nausea
- Constipation
- Diarrhoea
- Black stool
- Flatulence - bloating
- Sweating
- Bloating - flatulence
- Indigestion
- Stool with blood - blood in the stool
- Muscle weakness
- Fatigue
- Vomiting
- Stuck winds - stopping the outflow of gases
- Yellowish skin
- Increased body temperature
Characteristics
It is a multifactorial disease process whose aetiology includes genetic factors, environmental exposures (including diet) and inflammatory changes in the digestive tract.
Invasive colorectal cancer is a preventable disease. Early detection through widely used screening programmes is the most important factor in the progressive decline of colorectal cancer in developed countries.
Causes
Some things in life simply cannot be controlled. The same is true for some factors in the development of colorectal cancer.
These factors can increase your risk of developing colorectal cancer:
- Age - The risk of colorectal cancer increases with age. Younger adults can get colon cancer, but it is much more common after age 50. But colorectal cancer increases among people younger than 50, and the reason remains unclear.
- Race and ethnicity - Colorectal cancer diagnosis and death rates are highest among non-Hispanic African Americans. These numbers are also higher among Native Americans, Alaska Natives, and Jews of Eastern and Central European descent.
- History of polyps or cancer - The risk is higher for those who have had colorectal polyps in the past. Especially if they were large, abundant, or had abnormal but noncancerous cells (dysplasia). The risk is also higher for a patient who has previously had colorectal cancer.
- Certain medical conditions - Inflammatory bowel disease (IBD, including ulcerative colitis or Crohn's disease) lasting more than 8 years or type 2 diabetes mellitus may increase the risk of colorectal cancer. Irritable bowel syndrome (IBS) does not seem to be associated with a higher risk.
- Certain genetic syndromes - Inherited disease increases the risk of this type of cancer. These include Lynch syndrome or polyposis syndromes such as familial adenomatous polyposis (FAP). Lynch syndrome (HNPCC) causes about 6% of all colon cancers. Researchers are investigating whether other gene mutations, such as BRCA1 and BRCA2 mutations associated with breast cancer, may also increase the potential risk of colorectal cancer.
- Family health history - If other family members have had colorectal cancer or polyps, the risk of developing colorectal cancer is higher. This is especially true for first-degree relatives (parents, siblings, children).
Risk factors that can be influenced
According to gastroenterology societies, 55 percent of colorectal cancer diagnoses are attributed to controllable lifestyle factors.
These include:
- Diet - The risk of colon cancer is higher in individuals who consume a diet high in fat, high in processed meat or red meat. Conversely, a diet rich in fruits and vegetables is protective. Also, a high intake of fiber is associated with a reduced risk of colorectal cancer.
- Drinking alcohol - Moderate to heavy alcohol consumption, but even moderate drinking can increase the risk of colorectal cancer. Men should limit themselves to two drinks a day and women to one drink a day.
- Weight - The risk of colorectal cancer is higher in people who are overweight or obese, especially men.
- Physical activity - There is a link between physical activity and colon cancer, but not rectal cancer. People who spend a lot of the day sitting or lying down may be more likely to develop colorectal cancer.
- Smoking - The International Agency for Research on Cancer has definitively stated that tobacco smoking causes colorectal cancer. About 12 percent of colorectal cancer cases are caused by current or former smoking.
- Preventive medications - Regular, long-term use of aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs) has been shown to reduce the risk of colorectal cancer. This is especially true for people under age 70 who are at a healthy weight. However, patients should first consult a doctor before using these medications.
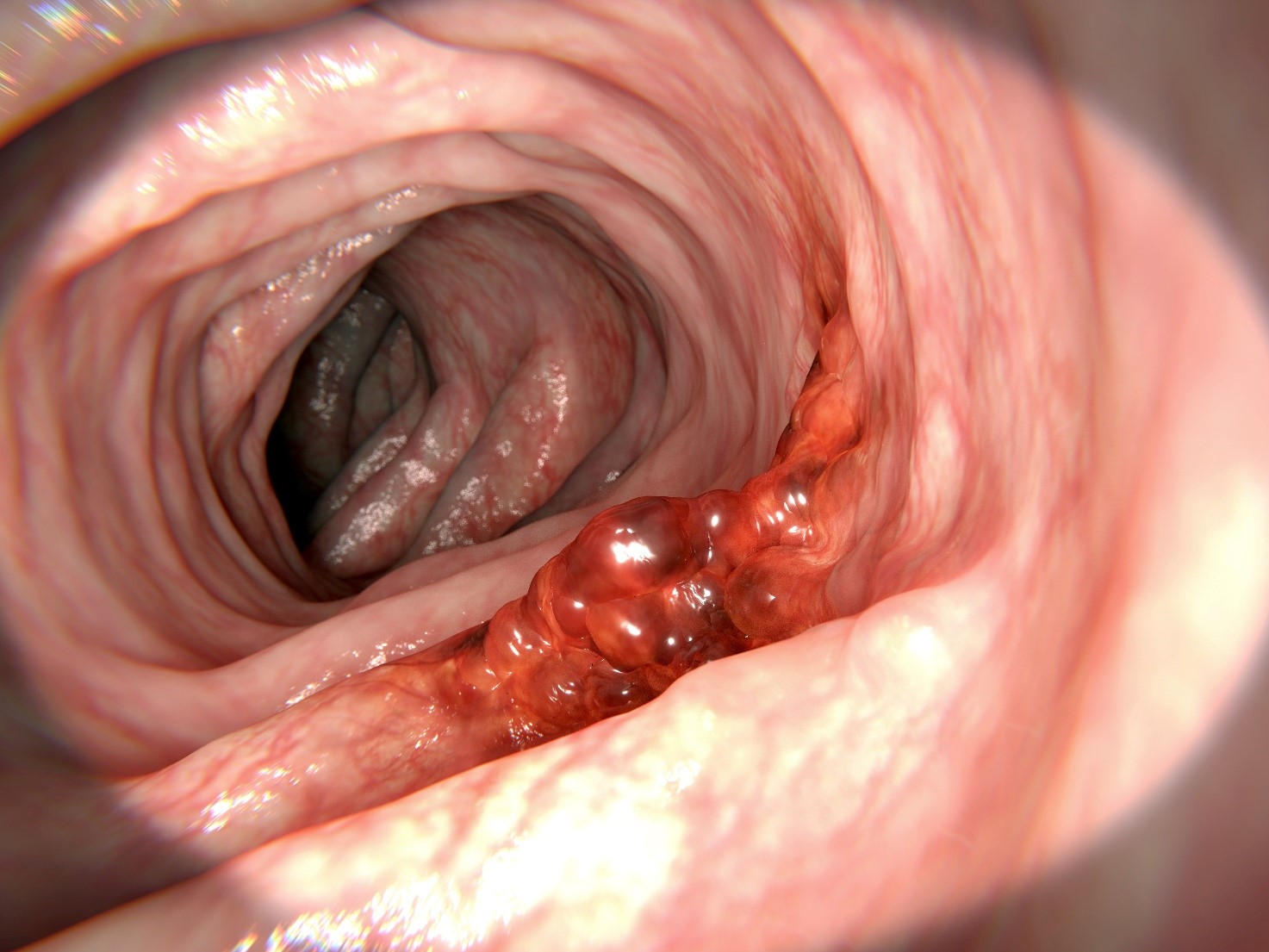
Colon polyps and the development of cancer
Colon polyps should be mentioned because they are precancerous. Polyps that become malignant give rise to carcinomas.
Polyps are growths from the lining of the colon that encroach on the lumen of the intestine. They are most commonly found as adenomas. They usually grow slowly - over several years (8-10 years).
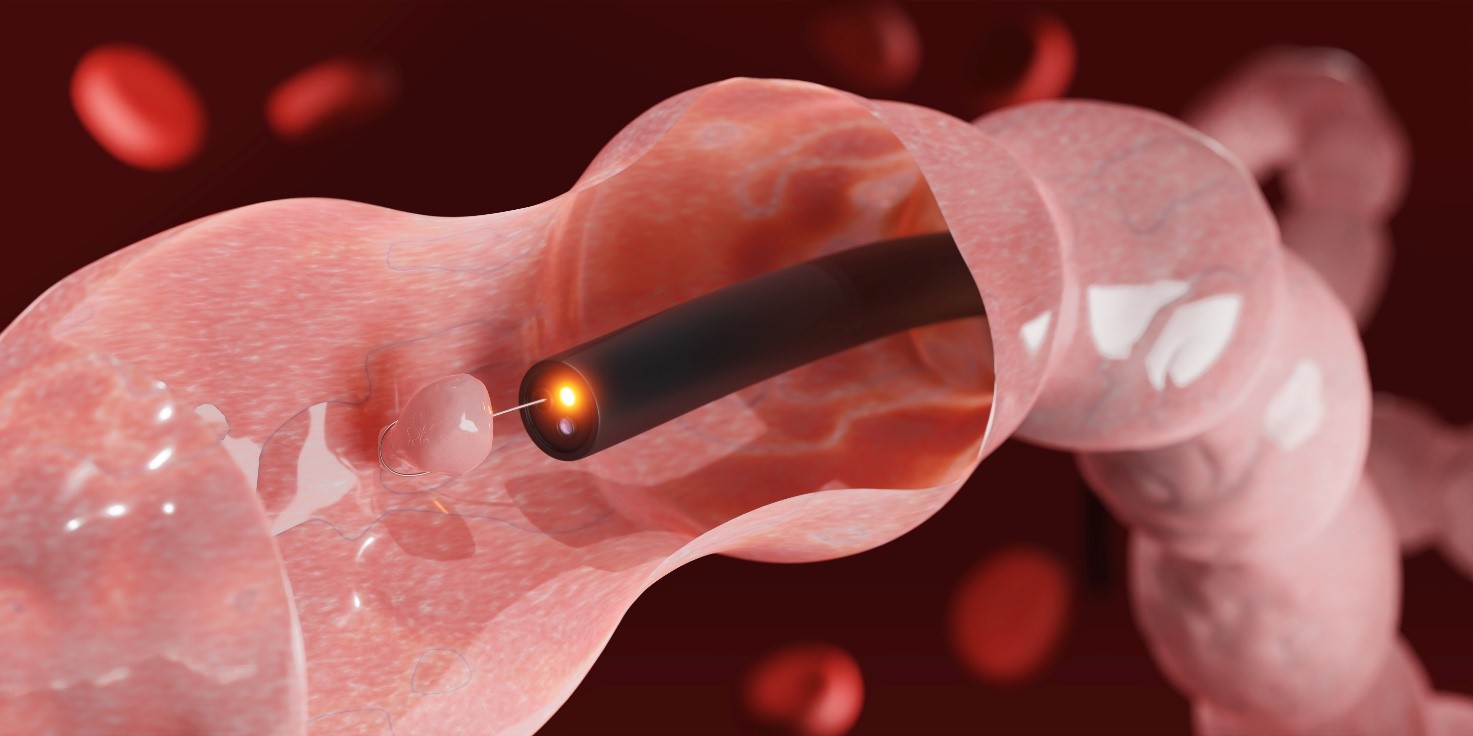
The preventive examination is precisely about finding and removing polyps. This can be done during a colonoscopic examination.
This turns a diagnostic colonoscopy into a therapeutic colonoscopy by means of an endoscopic polypectomy (removal of polyps). At the same time, colon cancer is prevented.
...so prevention is possible!
Symptoms
- changes in bowel habits
- diarrhoea or constipation
- a feeling that the bowel is not emptying properly
- blood in the faeces, making it look dark brown or black
- bright red blood from the rectum
- abdominal pain and bloating
- a feeling of fullness, even if it has been a long time since eating
- fatigue
- unexplained weight loss
- anaemia
For any of these symptoms you should see a doctor and consider having a colonoscopy.

Diagnostics
Physical examination and medical history
An examination of the body to check for general health symptoms, including checking for signs of illness such as lumps or anything else that seems unusual. A history of the patient's health habits, past illnesses, treatments, and family history will also be taken.
Digital rectal exam
Rectal examination. The doctor inserts a lubricated, gloved finger into the rectum to palpate for lumps or anything else that doesn't belong there.
Fecal occult blood test (FOBT)
A test to check the stool for the presence of blood that can only be seen with a microscope. A small sample of stool is placed on a special card or in a special container and returned to the doctor or lab for testing. Blood in the stool can be a sign of polyps, cancer, or other medical conditions.
The test for occult bleeding has low diagnostic value. Its negativity does not indicate the absence of a tumor.
Blood tests
Laboratory findings in the disease are not specific. People with colon cancer may or may not have anaemia. Oncomarkers may be elevated in CEA (carcinoembryonic antigen), CA 19-9 and rarely CA 125.
Irrigography
Irigography is an X-ray examination of the colon in which a barium contrast agent is injected into the rectum through a thin tube. The abdomen is then X-rayed and an image of the colon is obtained. The result of the examination is a visualisation of the lining of the colon and its irregularities, which may indicate a polyp, tumour or inflammatory disease.
The examination has recently been abandoned because of the radiation burden on the patient and the inability to accurately diagnose and intervene if necessary. Intervention is possible during the colonoscopic examination, which replaces this examination.
Sigmoidoscopy
A procedure to detect polyps, other abnormalities or cancer within the rectum and sigmoid (esophageal) colon. The colonoscope is inserted through the rectum into the esophageal colon.
The colonoscope may also have an instrument to remove polyps or take tissue samples to be examined under a microscope for the presence of cancer.
Colonoscopy
An examination to detect polyps, abnormalities, or cancer within the rectum and the entire colon. The examination is performed after the bowel has been prepared (emptied) with a laxative and a one-day fast. It is performed by a board-certified gastroenterologist or surgeon.
The examination can be performed without medication, under light sedation or general anaesthesia. During the examination, polyps can be removed or tumour samples can be taken for histological examination.
Virtual colonoscopy
A procedure that uses a series of X-rays called computed tomography to take a series of pictures of the colon. A computer combines the images to produce detailed pictures that may show polyps and anything else that appears unusual on the inside surface of the colon. This test is also called colonography or CT colonography.
The disadvantage of the test is the inability to remove pathological tissue and take a tissue sample.
Biopsy
A biopsy is the taking of a sample of pathological tissue for histological examination under a microscope by a pathologist. It is always a necessary part of the diagnosis of colon cancer.
Stages of colon cancer
Stage 0 - Carcinoma in situ, where the cancer cells do not extend beyond the lining of the colon or rectum.
Stage I - The tumor has grown from the lining to the muscle layer of the colon or rectum.
Stage II - The tumor has grown into the wall of the colon or rectum but has not yet spread to the surrounding tissue and lymph nodes.
Stage III - The tumour has spread to the surrounding lymph nodes. We are talking about locally advanced disease.
Stage IV - Disease has spread to distant organs. Secondary foci of disease - metastases are present.
Studies from 2019 suggest that many cancers metastasize before the original tumor can be detected by conventional screening methods. This is very unfavorable. This is also why the first sign of the disease is often the finding of metastases.
However, usually carcinomas metastasize later in the course of the disease.
Colorectal cancer metastasizes to the liver. This can be manifested by abdominal pain below the first rib arch, as elevated liver parameters in the biochemical picture from the blood. Metastases are visible on ultrasound, or CT scan, PET-CT (positron emission tomography combined with CT), on MRI. In case of unclear findings, biopsy of the liver lesions is available.
Metastases in the liver are often the first finding of the disease. Pulmonary metastases are seen as difficulty breathing, sometimes chest pain and a characteristic radiographic picture. They are also seen on CT, PET-CT and MRI scans.
How it is treated: Colon cancer
What is the treatment for colon cancer? Surgical, oncological
Show moreInteresting resources










