- tvojesrdce.sk - Slovak Heart Foundation - life after heart attack
- solen.sk - acute myocardial infarction - principles of current management
- techmed.sk - NSTEMI heart attack and unstable angina
- techmed.sk - STEMI heart attack
- alphamedical.sk - myocardial infarction - recapitulation of findings
What is life like after a heart attack? Does it limit, cause incapacity for work?
Diseases bring with them various limitations, and not only during their duration. Some diseases and conditions require a permanent change in lifestyle. Myocardial infarction is one of these conditions. Just because someone has overcome it does not mean that they will continue to live as they have been living. The aim is to prevent a recurrence of the disease, which is more likely with each successive heart attack in life. It is therefore necessary to change some habits or bad habits that may have been established.
Article content
Underestimation of the symptoms, unjustified waiting for them to disappear or a large infarction with damage to major or multiple heart vessels causes permanent consequences and limitations for the rest of life.
What does a myocardial infarction mean?
For a better understanding, two terms need to be specified. Heart attack and myocardium.
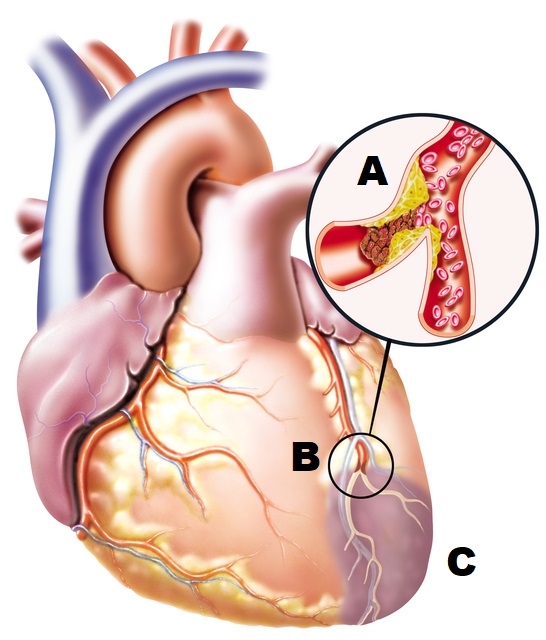
A heart attack means blockage of a blood vessel and its subsequent obstruction. The obstruction may be a blood clot, embolus or fat droplet, for example. Any blood vessel in the body may be affected. Depending on the location, a heart attack is divided into myocardial infarction, cerebral infarction, renal infarction, eye infarction and others.
- A partially obstructed (clogged) blood vessel has a narrowed lumen (translucency, diameter). The blood supply to the organ it previously nourished is restricted.
- Complete obturation prevents blood access to the organ or part of it and it dies.
The myocardium is the muscle of the heart. It forms the middle layer of the heart. It is surrounded on the inside by the endocardium (the inner lining of the heart). On the surface it is covered by the epicardium, which passes into the outer lining of the heart (the pericardium).
The blood supply to the heart - the coronary circulation
The blood vessels that supply the heart muscle are called the coronary arteries (lat. arteria coronaria cordis). They branch off from the heart wall (aorta) and have two main branches, the right and left (dextra et sinistra). These branch off into smaller arteries in the heart to supply blood and oxygen to the whole myocardium.
Pathophysiology of heart attacks: what happens in the heart after a blockage
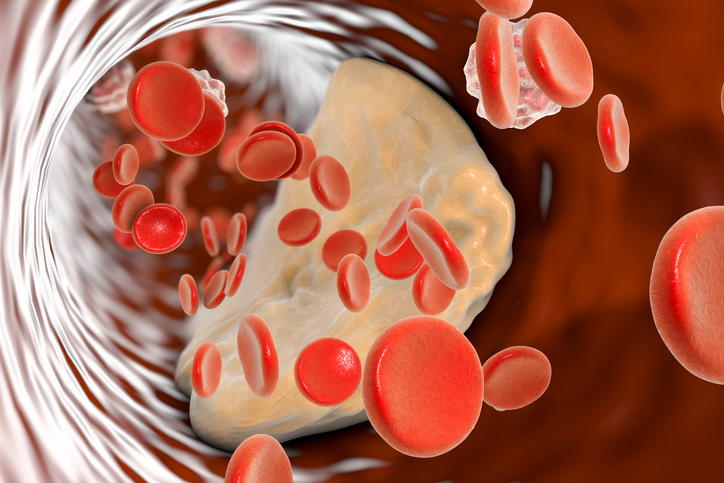
A blood clot can form directly in the heart or in another part of the body. Diseases of the veins of the lower limbs (e.g. inflammation, varicose veins), where clots are most likely to form, are a serious factor. They break off and travel through the bloodstream when there is a sudden movement. They stop only at the point of narrowing of the vessel, through which they cannot pass. They form an obstruction.
Clot formation can also be the result of an unhealthy lifestyle (smoking, alcohol, drugs and steroids in young people, stress, unhealthy diet). Factors that promote clot formation combine to increase the risk.
Thrombi (blood clots) can reach the coronary arteries of the heart, but also the lungs (lung infarction), the brain (stroke - apoplexy), the kidneys (kidney infarction) and any part of the human body.
The organ or part of the organ that was previously supplied by this blood vessel is not nourished by blood or oxygen. It gradually dies. This process takes several hours until the organ or part dies completely and irreversibly. Therefore, time plays a role in the treatment of a heart attack. The sooner the clot is dissolved, the less the health consequences and permanent damage.
The risk of thrombosis is increased by atherosclerosis. Atherosclerosis is a disease of the blood vessels that develops silently and without warning signs. It is sometimes detected only after a heart attack has occurred. It is damage to the inner lining of the blood vessels due to. Fat is easily trapped on the damaged endothelium. Elevated cholesterol is therefore a risk factor for its development. The trapped fat particles narrow the blood vessel, thus creating an ideal environment for the thrombus to attach.
Interesting:
The number of heart attacks is steadily rising. However, deaths from heart attacks are decreasing every year due to advances in medicine.
Treating heart attacks - time is of the essence
Treatment of heart attacks is carried out in specialized medical facilities. These facilities are equipped both in terms of personnel and technology to treat acute conditions associated with heart diseases.
This includes myocardial infarction, but also other serious heart conditions, such as heart rhythm disorders requiring the implantation of a pacemaker (in the case of high heart rate arrhythmias, for example, fibrillation) or a cardioverter (in the case of low heart rate arrhythmias, for example, stage III AV block).
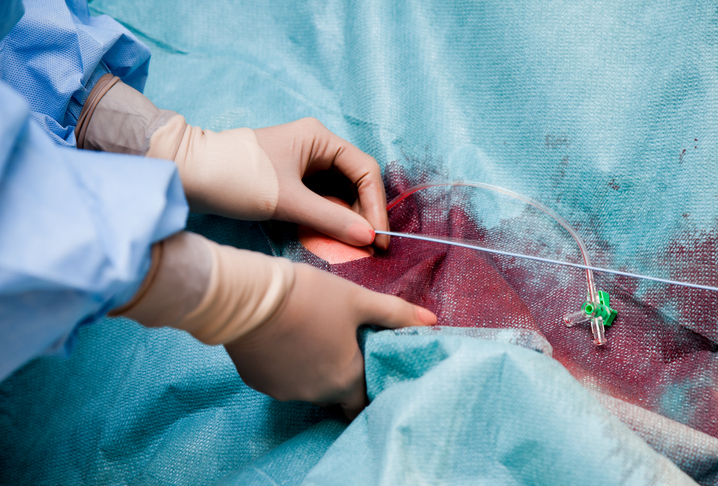
The golden hour
The so-called "golden hour" is a concept well known among cardiologists, but also physicians and first-responder healthcare professionals (emergency services). It is the time horizon from the onset of the first symptoms of myocardial infarction to the administration of treatment or other intervention (thrombectomy, stent) in one of these specialised centres.
Why is this time so important? Within one hour, the heart muscle is not damaged, despite the prevention of blood and oxygen supply. Its gradual death begins after one hour. Therefore, if the treatment of the infarction is started within the time window, the patient's condition is reversible. The remedy in this case is ad integrum (lat. completely or totally).
The patient survives, without any consequences or limitations.

The emergency services and the above-mentioned departments communicate and consult with each other by telephone, telemetry (sending ECG recordings) or by means of a mobile app.
You might be interested in:
For example, the Stemi Stroke app is very widespread. It is an app on the emergency services' mobile phone, in which an ECG recording is taken and sent to the nearest specialised workplace. The app assesses, by kilometre, which workplace is closest and colour-codes the possible occupancy. At the final workplace, they automatically receive the message. If necessary, the cardiologist can contact the ambulance crew in case of any questions (time of arrival and time to prepare the operating theatre). If the workplace is too far away, a helicopter ambulance service can be activated via the dispatching system, because of the time benefit for the patient. This collaborative system improves the possibilities and minimises the time window in the treatment of heart attacks.
Time window of up to three hours
Patients often unknowingly underestimate the symptoms of a heart attack. They attribute chest pain to spinal problems or other illnesses. As time passes, the patient misses the opportunity to treat ad integrum. Treatment within three hours of the onset of symptoms may leave no or minimal effects, usually without limitations. The limitations imposed are mainly related to prevention, through dietary modification and elimination of habits (smoking).
It is essential to know the symptoms of myocardial infarction and to call for help in time. For example, chest pain is a typical symptom, but it can also occur with other trivial problems. The table below shows the basic differences between cardiac and non-cardiac symptoms. The presence of each symptom may not be the same for everyone. However, chest pain, a feeling of lack of air, sweating and nausea are almost always present.
Interesting:
Some myocardial infarctions, especially those affecting larger or multiple vessels, are sudden. The patient falls unconscious before help can be summoned. Such severe conditions usually end in failure of resuscitation and death.
Sometimes the only symptom is dizziness and collapse.
The absence of chest pain is typical in diabetics. A heart attack is manifested by pressure in the stomach, pain, nausea, vomiting, marked pallor, sweating and dizziness.
Table of basic differences between cardiac and non-cardiac symptoms
| Cardiac symptoms | Non-cardiac symptoms | |
| Onset of trouble | Sudden without prodromes, often after physical exertion | gradual onset with prodromes |
| State of consciousness | dizziness, drowsiness, collapse, unconsciousness | full consciousness, dizziness |
| Breathing | Dyspnoea (shortness of breath), subjective sensation of lack of air, objectively choking person with presence of restlessness typical of choking | subjectively difficult in relation to breathing and movement, rapid breathing (hyperventilation) |
| Patient position | orthopnoic - patient forces a sitting position, usually with legs lowered, elbows resting on the mat (table), in a slight prone position to facilitate breathing | varies, sometimes the subjective feeling of not being able to breathe is improved when walking |
| Facial colour | distinctly pale, sometimes bluish lips, earlobes, fingertips | pale, red (no blue colouration) |
| Localisation of pain | centre of the chest between the nipples | anywhere on the chest |
| Radiation of pain | to the back of the shoulder blades or shoulders, neck and head, limbs, stomach | without radiation |
| Intensity of pain | severe to twinging | mild to moderate |
| Character of pain | pressure on the chest, burning, pinching, feeling of a heavy object on the chest | mostly stinging, sometimes pressure |
| Duration of pain | pain persists, does not improve without treatment | in attacks, sometimes persisting and changing in intensity |
| Factors aggravating the pain | Any physical exertion, talking | particular position, breathing |
| Neurological symptoms | dizziness, disturbances of consciousness, unconsciousness, tingling in some upper limb (usually the left upper limb) or just the fingertips, tingling around the mouth and tongue | dizziness, tingling in both upper or lower limbs |
| Vegetative symptoms | marked sweating (cold, sticky sweat), nausea, vomiting | sometimes sweating, mild nausea |
| Presence of significant anamnestic data | Significant pre-existing medical conditions (heart disease, high blood pressure, clotting problems, venous inflammation, diabetes) or recent heart attack | spinal disorders, migraines, hyperventilation tetany, psychological illness, stress, trauma, injury, exhaustion |
After a time window...
Sometimes it happens that a patient is brought to a specialized facility after the time window. This may be due to his late request for help, long arrival time to the hospital (long kilometre distance, non-airworthiness of the helicopter ambulance service or night hours when the helicopter is in night mode and the preparation for take-off to be safe is 45 min).
After the time window, irreversible damage to the heart muscle occurs, which brings with it consequences. The severity of these, of course, depends on several factors, such as the site of myocardial damage, the severity of the myocardial damage, the size of the damaged area and the patient's previous medical condition.
In most cases, they involve weakening of the heart wall, disturbances in the transmission of nerve impulses in the heart and the development of a wide range of heart rhythm disturbances. There may be a reduction in the ejection fraction of the heart and heart failure.
These consequences already bring limitations.
Consequences and limitations in life after a myocardial infarction
As mentioned above, the consequences depend on the size of the heart involvement, the time window and speed of initiation of treatment, as well as the general health and age of the patient. Involvement of small vessels and parts of the heart muscle with treatment in the window heals ad integrum without permanent consequences. Larger infarcts, previous heart disease and late treatment are a problem.
Although part of the heart muscle dies, the rest of the muscle functions normally. Shortly after a heart attack, its performance is reduced. With small damage, it heals over time and the heart's performance increases. The time for full recovery after a heart attack is one to two months.
In large infarctions, the heart's performance remains permanently reduced. The dead muscle heals with a scar. But the scar can never replace the original tissue. The heart is more sensitive to stress and the blood pumping function may be impaired. Blood stagnates in both the small and large blood circulations, putting strain on the heart and lungs and causing heart failure.

Restrictions also apply to diet and obesity reduction
Fat restriction - One of the causes of a thrombus attaching to a coronary vessel is atherosclerosis. This occurs as a result of obesity or elevated cholesterol. The damaged heart is extremely sensitive and overloading it with a diet full of fat is not advisable. Obesity and elevated cholesterol continue to damage the heart and blood vessels, impairing its already reduced function.
It is scientifically proven that a high BMI index causes high blood pressure. Arterial hypertension is a risk factor for recurrent heart attacks, aggravates coronary heart disease, arrhythmias and contributes to the worsening of the development of heart failure.
Salt restriction - Impaired pumping of blood results in stagnation of blood in the small and large bloodstream. This causes fluid to accumulate in the heart and lungs. The fluid in the lungs is called pulmonary edema (swelling) - layman's term for water on the lungs. Lungs full of fluid cause breathing disorders to the point of the patient suffocating and dying. Fluid in the heart prevents its proper function and causes it to fail. Salts retain water in the body, worsening this condition. Therefore, cardiac patients and people after a heart attack should avoid over-salted foods.
Pulmonary oedema and heart failure are manifested by respiratory disturbances. The patient suffocates. The colour of the face changes from pale to waxy to ashy, bluish to blue. The blue colouring starts on the acral parts such as the lips, mucous membranes, earlobes and fingertips. As the condition progresses, the patient turns blue all over the face. When breathing, moist phenomena are heard at a distance, grunting. The sound can be compared to the sound coming from a glass of water when blowing into it with a straw (gurgling).
Interesting:
Scientific studies in France have shown no effect of salt on the development of arterial hypertension. Experts have analysed its effects on up to 8670 people.
Limit sugars - Sugars are the worst for heart function. They even have a worse effect on clogging and damaging blood vessels, developing arterial hypertension and causing recurrent heart attacks than fats. Triglycerides may be to blame. People who consume more than the recommended daily intake of sugars have up to twice the risk of recurrent heart attacks.
People who have had a heart attack should be much more careful. Their blood vessels are usually damaged by the atherosclerotic process, and excessive intake of sugars could make this condition worse. They should especially avoid excessive sweetening, sweets and sugary drinks. One can of sweetened drink contains between 30 and 40 g of sugar (about 5 teaspoons of granulated sugar).
Beware of fluids - As early as the 6th century BC, Thales said, "Without the circulation of fluids there would be no life." And he was right. Man is made up mostly of water and depends on a constant supply of it throughout his life. Fluids thin the blood and thus prevent the risk of blood clots. If patients do not follow a drinking regime, they are at risk of a repeat heart attack.
Important:
Elderly people who have heart failure take medication to drain their blood.
This forces them to go to the toilet all the time, which makes them understandably fed up. Therefore, some may either come off the medication or start drinking too little.
Neither solution is correct.
Coming off the medication can cause heart failure, and lack of fluids increases the risk of thrombus formation.
A heart damaged by a heart attack and failing is paradoxically very sensitive to fluid overload. Some lifers take diuretics - drugs to drain just to prevent heart failure overload as a pump. This does not mean they should cut back on drinking. However, it is not advisable to drink half a litre of fluid at once and quickly.
They should take fluids in smaller amounts and more frequently.
Physical activity is important, but in moderation
Physical activity and sport is good for health.
It aids in the metabolism and breakdown of fats and sugars. It prevents obesity and hypertension and reduces the amount of fat in already obese patients.
Excessive exertion in gyms or at work, on the other hand, can be harmful.
Excessive activity in people who have had a heart attack causes a transient increase in blood pressure, heart rate, and risk of arrhythmia to fibrillation.
In coronary heart disease, which is very often diagnosed in connection with a heart attack, there is excessive narrowing of the coronary vessels, insufficient blood supply to the heart and symptoms identical to those of a heart attack.
Naturally, this disease increases recurrent heart attacks. With excessive physical activity, it even causes and accelerates cardiac insufficiency and the development of pulmonary oedema. The condition progresses rapidly and often ends in death.
Patients who have had a heart attack should by no means avoid walking and sporting activities. However, everything should be done in moderation and not run a marathon. Some people, however, should minimise physical activity to the lowest possible level. These are those who have had repeated heart attacks, have chronic heart failure with a low ejection fraction and are therefore at high risk. Even the slightest exertion can put them at risk.
The length of disability depends on several factors, the extent of the heart attack or early diagnosis and treatment. Of course, it also depends on the person's general condition.
A doctor should be alerted to such a serious condition.
Forget about past habits
Habits are detrimental to health on several levels. They are not beneficial to health, but we are still subject to them. Addiction to these substances is to blame. These include smoking, excessive consumption of caffeinated drinks, alcoholism, drug abuse and, increasingly these days, steroid use.
Nicotine causes constriction of blood vessels, including coronary vessels, and ischemia of the heart muscle. This results in chest pain. Together with other substances in the cigarette, it increases the risk of blood clots. Women who smoke and take contraceptives, which have a similar effect, are particularly at risk. Also male smokers who succumb to the desire for a perfect body and inject steroids.
Alcohol, on the other hand, dilates blood vessels, forcing the diseased heart to work faster and pump potentially insufficient blood circulation. It causes the heart to beat faster and increases the risk of arrhythmias. Of course, its destructive effect on blood vessels and the whole body is also well known.
After a heart attack, permanent treatment and regular cardiological checks
A diseased heart belongs in the hands of a doctor. After suffering a serious myocardial infarction, consequences can remain, which is why it is necessary to attend regular check-ups at the cardiology outpatient clinic. There, it can be detected early on whether the condition is improving, responding to treatment or progressing.
At the outpatient clinic, the doctor spins an ECG, which can pick up various changes in the heart's function. Blood pressure is also measured, which could increase the risk of a recurrent heart attack. Blood is also taken for laboratory tests. Elevated cholesterol or its consistency and density, which can cause recurrent clot formation, can be detected early in the blood.
Patients have to take medication permanently after overcoming a heart attack. Almost everyone takes blood thinners such as aspirin, warfarin, prasugrel, clopidogrel and other preparations. Depending on the condition, they are given medication for high blood pressure (antihypertensives), drugs to support heart function and drainage, or cholesterol medication.
Interesting resources










