- ncbi.nlm.nih.gov - Myasthenia Gravis, Beloor Suresh A, Asuncion RMD.
- ncbi.nlm.nih.gov - Myasthenia Gravis: A Review, Annapurni Jayam Trouth, Alok Dabi, Noha Solieman, Mohankumar Kurukumbi, and Janaki Kalyanam
- mayoclinic.org - Myasthenia gravis
- my.clevelandclinic.org - Myasthenia gravis (MG)- Cleveland Clinic
- solen.sk - MYASTHENIA GRAVIS IN THE AMBULANCE OF YASTHENIA GRAVIS IN THE AMBULANCE OF PRACTICE, Peter Špalek, Centre for Neuromuscular Diseases, Neurological Clinic SZU, FNsP Bratislava - Ružinov
- solen.cz - Myasthenia gravis, MUDr. Jiří Pitiha, Centre for Myasthenia Gravis, Neurological Clinic of the 1st Faculty of Medicine, Charles University in Prague, Centre for Clinical Neurosciences, Neurological Department of KZ a.s. - Nemocnice Teplice o. z., Teplice
Myasthenia gravis: What it is and what are its symptoms + Causes

Myasthenia gravis is a relatively rare autoimmune disease affecting the neuromuscular junction. It manifests itself as fluctuating muscle weakness, which can affect, among other things, important respiratory muscles. It can lead to a so-called myasthenic crisis, an urgent and life-threatening condition.
Most common symptoms
- Malaise
- Speech disorders
- Hoarseness
- Spirituality
- Double vision
- Defence
- Falling eyelids
- Swallowing disorders
- Muscle weakness
- Fatigue
- Vomiting
Characteristics
Its incidence is 200 cases per 100,000 population, making it a rare disease. However, most physicians will encounter it in their practice.
The disease most often affects young women or older men.
Childhood MG is relatively rare in the Western world, occurring mainly in Asian countries, where approximately 50% of patients are under the age of 15.
Its typical manifestations include fluctuating muscle weakness, which is more pronounced in the afternoon and after exertion. Conversely, symptoms are absent in the morning and after rest.
It usually affects the eye, neck and limb muscles.
In children, it is mainly manifested by symptoms of weakness of the extraocular muscles.
Causes
The neuromuscular disc is where the nerve endings connect to the muscle fibres. This connection ensures the transmission of electrical impulses from the nerves to the muscles.
The connection of nerves to each other or nerves to muscles is called a synapse. A special kind of synapse is also a neuromuscular disc.
A specific chemical called acetylcholine is secreted from the nerve into the gap between the nerve and the muscle. Acetylcholine binds to its receptors on the muscle fiber and starts a cascade of chemical reactions that lead to muscle contraction.
This is how all movement in our bodies is controlled.
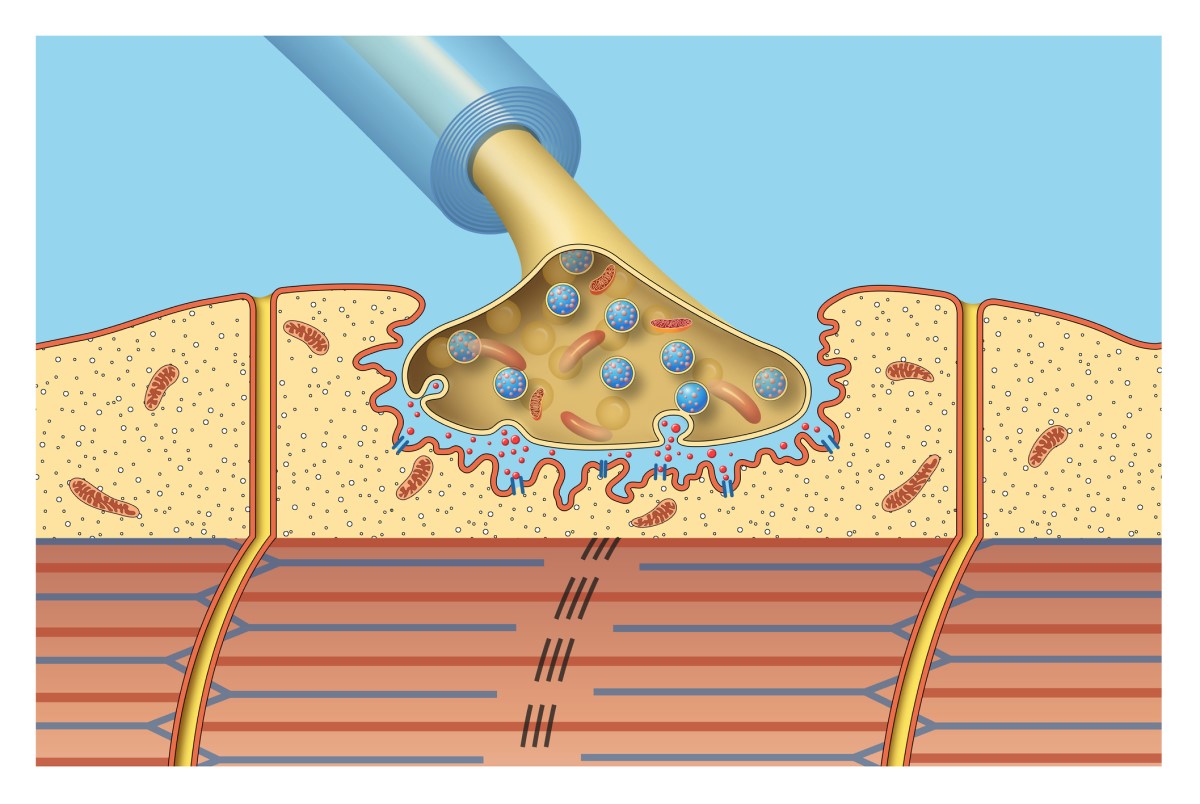
In myasthenia gravis, autoantibodies, or immune antibodies, are produced against the body's own tissues.
These autoantibodies occupy up to two adjacent acetylcholine receptors, reducing the capacity and functional reserve for adequate neuromuscular transmission.
Furthermore, immune processes are activated, leading to the destruction of the postsynaptic membrane on the muscle. This completely disables the neuromuscular transmission process.
This means that the information about the movement is transmitted correctly by the nerves, but it no longer reaches the muscles. Therefore, the movement is ultimately not carried out.
Approximately 80% of people with MG test positive for the presence of these specific autoantibodies.
In young individuals who become ill before the age of 45, the thymus plays an important role in the development of MG.
The thymus gland (also known as the infant gland) is the primary immune organ in which T-lymphocytes are formed in childhood. It is located in the thorax and its size changes with age.
In children, it is the largest and reaches a size extending from the thyroid gland to the heart. It shrinks with age and turns into adipose tissue. In adulthood, it is small. It is located behind the sternum and has an irregular shape.
In some people, hyperplasia of the thymus may occur, that is, the growth of its cells and its enlargement.
On the surface of these so-called myoid cells are proteins similar to the acetalcholine receptor (AChR). These are recognised by T-lymphocytes as foreign and an autoimmune attack is launched against them.
This results in autoimmune inflammation with activation of both T-lymphocytes and B-lymphocytes and production of autoantibodies.
In addition, other proteins are found in the muscle, such as the structural protein 'muscle specific tyrosine kinase' (MuSK).
Antibodies to this protein and to some other structures on the postsynaptic membrane have also been found in some patients with myasthenia gravis.
MuSK in myasthenia gravis has clinical features that are quite different from myasthenia gravis with other autoantibodies. It is more common in women. It relatively spares extraocular muscles and commonly affects bulbar, facial and neck muscles.
Myasthenic crisis is also common in MuSK MG.
Approximately 13% of patients have myasthenia associated with an ongoing malignancy. At that time, myasthenia is referred to as paraneoplastic. Most commonly, it is a thymoma, which is a benign tumor of the thymus.
Myasthenia is an autoimmune disease. Therefore, it often occurs in association with other autoimmune diseases, such as autoimmune thyroiditis.
Classification of myasthenia gravis
Depending on the type of clinical symptoms and the type of autoantibodies, MG can be classified into different subgroups.
Each group responds differently to treatment and therefore has a different prognosis:
- MG with early onset - Age at onset of symptoms is less than 50 years, associated with thymic hyperplasia.
- MG with late onset - Age at onset of symptoms is greater than 50 years and is associated with atrophy (shrinkage) of the thymus.
- MG associated with thymoma
- MG with anti-MuSK antibodies
- Ocular MG - Symptoms from the oculomotor muscles only
- MG without detectable antibodies to AChR and MuSK
Symptoms
Most commonly, several muscle groups are affected. Monofocal involvement (involvement of only one muscle group, for example only the muscles of the eye) is not uncommon.
The most common symptoms include the following:
extraocular muscle weakness
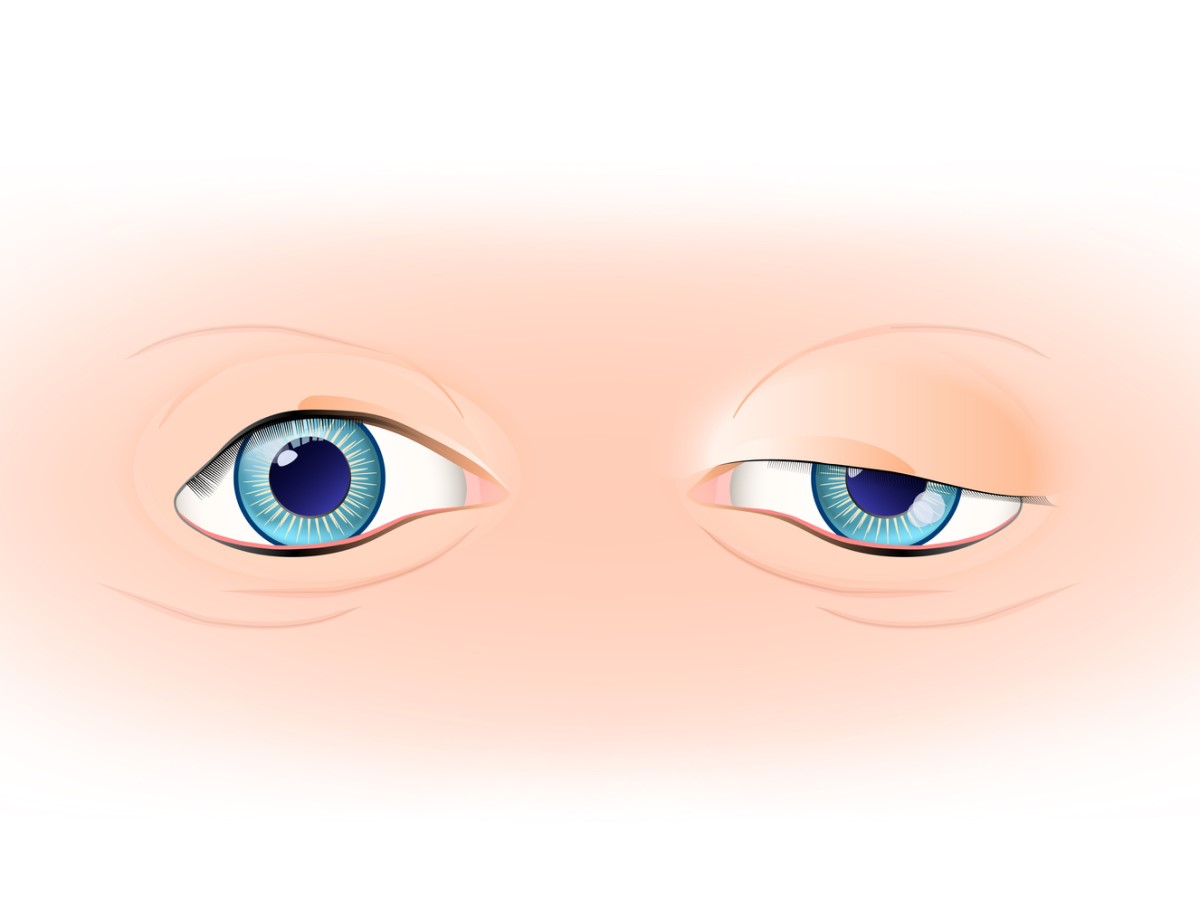
In approximately 85% of patients, this is the initial symptom signalling myasthenia gravis. Patients suffer from double vision (diplopia), drooping of the upper eyelid (ptosis) or a combination of both.
These symptoms can progress to 'generalised MG', which already involves the bulbar, axial and limb muscles. Half of patients develop this form within two years.
Weakness of the bulbar muscles
These are symptoms such as difficulty chewing solid food or frequent gagging and choking. There is also difficulty swallowing, hoarseness and poor articulation when speaking.
Impaired mobility of the facial muscles causes an expressionless face, without facial expressions. Impairment of the neck muscles causes drooping head syndrome.
Limb weakness
Weakness affects several groups of so-called proximal muscles (muscles closer to the middle of the body), such as the shoulders and thighs. The upper limbs are more severely affected than the lower limbs.
Myasthenic crisis
Myasthenic crisis is the most serious symptom of this disease.
It is a disorder of mobility of the intercostal muscles and diaphragm.
These muscles help to expand the lungs when breathing in. If they remain immobile, the lungs do not expand and the patient cannot breathe.
This is a life-threatening condition. A patient in myasthenic crisis must be admitted to the intensive care unit with the need for artificial pulmonary ventilation.
Diagnostics
Neurological examination
Sometimes neurological examination of muscle strength may not reveal any disorder. This is due to the fluctuating nature of the disease.
In such cases, repeated or sustained muscle contractions may demonstrate weakness. For example, looking up for at least 1 minute will highlight ptosis of the upper eyelid, i.e. its downward droop.
Improvement occurs after a period of rest or after application of ice, also referred to as the ice pack test, to the affected muscle group.
In the medical history, the doctor asks about having an infectious disease, stress, increased fatigue or taking certain medications. All these factors can be a trigger for myasthenia gravis or can worsen previously only mild symptoms.
Serological tests
The serological test for the presence of autoantibodies to the acetylcholine receptor (Anti-AChR) is a very specific test that virtually confirms the diagnosis in patients with classic clinical findings.
It is positive in four-fifths of cases in patients with generalized MG, but only in half of patients with the purely ocular form of MG.
The rest of the patients, approximately 5-10%, have positive antiMuSK antibodies.
Only rarely are antiAChR and antiMuSK antibodies present in the same patient.
Some patients are not positive for either of these antibodies. Other types of antibodies may be tested in these patients, which is relatively rarer. A certain percentage remain without detection of a specific antibody. These patients have so-called seronegative MG.
Electrophysiological tests
This test is most beneficial in patients who are seronegative on antibody testing.
The most commonly used tests to determine MG are the repetitive (repeated) nerve stimulation test and single fiber electromyography (SFEMG). Both tests assess conduction delay in the neuromuscular disc.
The repetitive nerve stimulation test is based on the principle that repetitive nerve stimulation depletes acetylcholine in the neuromuscular disc. This gradually reduces the potential for electrical impulse propagation. A decrease of at least 10% is a diagnostic sign of MG.
Edrophonium test
Edrophonium is a short-acting acetylcholinesterase inhibitor. Acetylcholinesterase is an enzyme that breaks down acetylcholine. Administration of edrophonium will increase the availability of acetylcholine in the neuromuscular disc in the short term.
This test is particularly useful in the ocular form of MG, where electrophysiological testing is not possible. A positive result is obtained if the patient shows an improvement in symptoms, e.g. ptosis (drooping eyelids) or double vision.
Ice pack test
If edrophonium testing is contraindicated, an ice pack test can be performed. An ice pack is applied to the eye for two to five minutes. Any improvement in ptosis is then assessed.
However, this test is not suitable for the evaluation of extraocular muscles, i.e. in double vision.
Imaging methods
To assess thymoma, computed tomography (CT) or magnetic resonance imaging (MRI) of the chest is performed.
If it is a purely ocular form of MG, MRI of the orbit and brain may be performed to exclude any local lesions.
Other laboratory tests recommended include antinuclear antibodies (ANA) to rheumatoid factor (RF) and baseline thyroid function tests. Other autoimmune diseases may be present along with MG.
The differential diagnosis of myasthenia gravis includes
- Lambert-Eaton syndrome is also characterised by fluctuating weakness, but this improves with exercise. This distinguishes it from MG.
The disease is usually caused by a primary malignancy, most commonly small cell carcinoma of the lung.
- Thrombosis of the cavernous sinus may present with persistent eye disorders such as photophobia (light intolerance), chemosis (swelling and swelling of the conjunctiva) and headache.
It usually has a sudden onset.
- Brainstem gliomas are malignant tumours. They present with bulbar symptoms (difficulty swallowing, speech etc.), weakness, numbness, balance problems and seizures. Symptoms are permanent, not fluctuating as in MG.
They also usually present with headaches and symptoms of increased intracranial pressure, e.g. vomiting.
- Multiple sclerosis can present with any neurological symptom. It can fluctuate or persist for hours, days or weeks.
It manifests itself as weakness, sensory deficit, thought and behavioural disturbances. Weakness may be unilateral or bilateral.
- Botulism manifests very similarly to the ocular form of MG, with ptosis, double vision, progressive weakness and pupillary abnormalities.
It is also accompanied by systemic symptoms. A history of ingestion of honey or contaminated food by the patient is important.
- Tick-borne diseases are manifested by ascending limb paralysis, respiratory distress and decreased reflexes caused by neurotoxins from tick saliva.
- Polymyositis and dermatomyositis are diseases that cause weakness of proximal muscles, similar to MG. They are also usually associated with pain in these muscle groups.
It is an inflammation of the muscle itself.
- Graves' ophthalmopathy is manifested by tightening of the eyelids. Symptoms are caused by autoantibodies directed against the structures of the eye.
Course
They may worsen due to previous infections, physical exertion, mental stress and exhaustion. They improve after rest and sleep. Such a fluctuating course is characteristic of the disease.
The majority of MG patients have a near-normal life expectancy with current therapy. Fifty years ago, the mortality rate in myasthenic crisis was around 50-80%. Now it has decreased substantially to 4.47%.
Various clinical, laboratory and imaging findings are also of prognostic importance in MG.
For example, the risk of secondary generalization increases with late age of onset, high acetylcholine receptor (AChR) antibody titers, and the presence of thymoma.
The presence of a combination of both ptosis and double vision at disease onset has a higher likelihood of secondary generalization compared with ptosis or diplopia alone.
Early treatment with immunosuppressive drugs such as corticosteroids and azathioprine significantly reduces the risk of secondary generalization of the disease.
How it is treated: Myasthenia gravis
Treatment of myasthenia gravis: medications and other measures
Show moreMyasthenia gravis is treated by
Other names
Interesting resources










