- revue.ederma.sk - Solar radiation and its effect on the skin
- prolekare.cz - Diagnosis of malignant melanoma using whole-body scanning
- prolekare.cz - Current trends and new treatment options for melanoma
- prolekare.cz - Cutaneous melanoma: diagnosis, treatment and postoperative follow-up
- prolekare.cz - Metastases in the skin
- prolekare.cz - A review of the influence of vitamin D receptor polymorphisms on the development and progression of malignant melanoma
- prolekare.cz - Targeted treatment of melanoma: fact or fiction?
Malignant melanoma: What are the symptoms and what does it look like? Forms, their prognosis

Malignant melanoma is the 19th most common cancer. It is one of the most aggressive cancers.
Most common symptoms
Characteristics
Nowadays we pay a lot of attention to our appearance. We take care of our hairstyle, eyebrows and nails. Taking care of our skin is also very important.
Skin care is not just about hygiene, regular moisturizing treatments or beauty treatments.
Many women and men find the time for a manicure, pedicure or eyebrow grooming. But who among us finds the time for a preventive check-up with a dermatologist?
European Melanoma Day is held in May. Screening and preventive examinations of moles are carried out.
In the past, melanoma was considered a rare type of cancer. Over the last 50 years, its incidence has risen faster than that of other cancers.
In 1970, an average of 3.2 new cases per 100 000 inhabitants were reported in men and 3.3 cases per 100 000 inhabitants in women. By 1990, this figure had risen to 8.1 new cases in men and 7.8 in women. The number of cases is still rising. Currently, the number of melanoma cases is around 15 per 100 000 inhabitants.
Melanoma is a malignant skin tumour arising from the malignant transformation of melanocytes. It can metastasize rapidly to the lungs, brain and heart. It is very insidious.
We often think of melanoma as a skin disease, but it can also arise on mucous membranes such as the mouth or genitals. In women, it is more common on the face and legs. In men, on the upper torso.
Malignant melanoma is mainly found in white people. It affects mainly middle-aged people. It is also increasingly common in younger people.
The incidence of melanoma in men and women depends on age. Under the age of 40, melanoma is more common in women than in men. Over the age of 65, it is twice as common in men as in women.
The incidence of malignant melanoma has been increasing in recent years, particularly in Australia, North America, northern Europe and New Zealand.
How does malignant melanoma arise?
Malignant melanoma arises from the malignant transformation of melanocytes. Melanocytes are the cells of the basal layer of the epidermis that make the pigment melanin. Normal melanocytes can be thought of as wandering cells.
During ontogeny (development of the individual) they wander to the sites where melanin is formed. They have no intercellular contact structures. After mitotic division they tend to separate.
Melanocytes are a prerequisite for the development of malignant melanoma. The development of the disease does not depend on melanogenesis (the process of melanin synthesis). This finding illustrates the development of the disease in albinos.
International Classification of Diseases (ICD-10) - C43 - Malignant melanoma of the skin, melanoma malignum cutis.
Causes
The causes of the disease are unknown. More than 50% of patients develop malignant melanoma on clinically normal skin. Unfortunately, these patients seek medical attention only when subjective symptoms appear.
The subjective symptoms of malignant development include:
- melanoma enlargement
- swelling
- bleeding
- itching
A further 5% of patients develop malignant melanoma due to lentigo maligna. This means that it arises in areas exposed to UV radiation.
Approximately 30% of patients develop malignant melanoma from a pre-existing mole.
Several factors significantly influence the incidence and characteristics of this disease. These factors include:
- hereditary influences
- increased exposure to UV radiation
- frequent sunbathing in a tanning bed
- phenotypic characteristics (skin and hair colour)
Approximately 10% of all melanomas are familial. Reduced skin resistance to harmful influences may be genetically determined.
Mutations of individual chromosomes and the inability to correct chromosomal changes play an important role.
TIP to article:
Beautifullytanned skin and our health: How to get a healthy tan?
One of the risk factors for melanoma is sunburn in childhood.
Children who have more than one sunburn before the age of 12 have a 3.6 times higher risk of developing melanoma.
In the following section, we briefly describe the positive and negative effects of sunlight. Sunlight has a large impact on the environment. It consists of visible (50%), infrared (45%) and ultraviolet (5%) radiation.
The ultraviolet (UV) part of the solar spectrum is very important for many processes in nature. It is divided into:
- UVA radiation - Causes skin aging.
- UVB radiation - Causes tanning and burning of the skin.
- UVC radiation - Virtually does not reach the earth's surface because it is filtered by the atmosphere.
What are the effects of ultraviolet radiation on our bodies?
In small doses, ultraviolet radiation is needed for the conversion of vitamin D in the skin. However, larger amounts of UV radiation cause various changes to the skin:
- acute - redness, inflammation, overheating
- subacute - photodermatosis
- chronic - photoaging, carcinogenesis
TIP to article:
Vitamin D and its effects. Our health, strong bones and strong immunity?
The most serious harmful effect of UV radiation is the risk of carcinogenesis. UV radiation slows down cell division, inactivates intracellular enzymes and induces mutations.
UV radiation is considered the most important factor in the development of melanoma and non-melanoma skin cancers. Personal factors play an important role in their development:
- skin type
- skin hydration
- type and dose of UV radiation
- age
- method of exposure
- anatomical positioning
Among the external factors, altitude, latitude, radiation reflection, wind, humidity and air temperature are important contributors to the development of the disease.
An example of a typical melanoma patient is an employee working in an office environment who is not regularly exposed to UV radiation. He regularly goes on holiday to the seaside. He also likes to relax by the sea in winter.
Repeated and unprofessional application of artificial sources of UV radiation (tanning beds with UVA source, application of UVA in the context of phototherapy) is considered to be one of the risk factors.
The use of sunbeds is very popular. Nowadays, everyone wants to be beautifully tanned all year round. In addition to beautifully tanned skin, we also take away several side effects from sunbeds:
- burning of the skin
- phototoxic reactions to drugs
- polymorphic light eruptions
- development or recurrence of porphyria
- induction of malignant melanoma
Regular sunbed users are three times more likely to develop melanoma than other people.

Among the risk factors, a person's phenotype is of great importance. The most risky types of people:
- light skin phototype (phototype I and II)
- light hair colour (blond, red)
- light eye colour (green, blue)
table: Characteristics of each phototype
| Phototype I |
|
| Phototype II |
|
| Phototype III |
|
| Phototype IV |
|
| Phototype V |
|
| Phototype VI | typical of blacks |
Symptoms
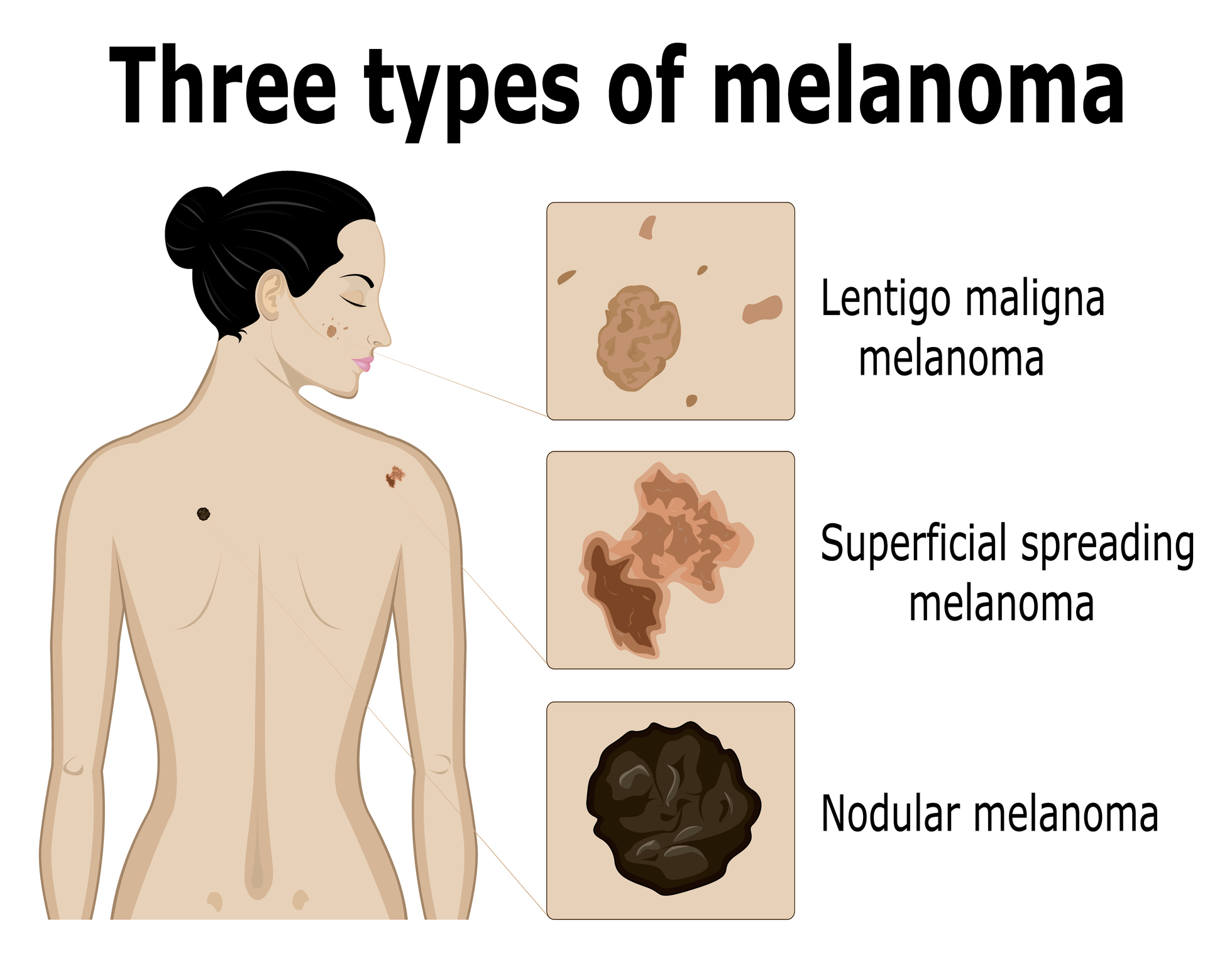
The following forms of malignant melanoma are distinguished:
lentigo maligna melanoma (LLM)
Lentigo maligna melanoma accounts for approximately 5 to 15% of cases. It occurs in older people (60-70 years). It is usually located on the head, neck and parts of the limbs exposed to the sun.
This type of disease is characterised by slow growth (5-20 years). It appears as irregularly pigmented and indistinct patches. Malignant transformation is characterised by the appearance of dark brown to black irregular pigmentations.
The prognosis is relatively favourable.
superficial spreading melanoma (SSM)
Superficial spreading melanoma is the most common type of melanoma. It accounts for 60 to 70% of all diagnosed melanomas of the skin. Most cases are diagnosed between the ages of 40 and 50.
In both sexes, it occurs mainly on the back. In women, it appears on the legs.
At the beginning, unevenly coloured lesions gradually form on the skin. It appears as a gradually enlarging macule or plaque. It is usually more than 6 mm in diameter.
This type of melanoma is characterised by different colours (brown, pink, grey, whitish).
nodular melanoma (NM)
Nodular melanoma is the second most common type of malignant melanoma. It accounts for 15 to 30% of all melanomas. It occurs between the ages of 50 and 60. It affects mainly men. It can occur mainly on the trunk and legs.
It grows rapidly on clinically unchanged skin.
It is a variably sized, irregularly pigmented hemispherical bump or papule. It has a smooth surface, does not peel, erodes rapidly and bleeds with minimal trauma. The colour may be brown, black or pinkish red.
Metastasis is rapid. It forms mainly in regional nodules, lungs, brain, liver, bone and skin. Prognosis is not favourable.
acral lentiginous melanoma (ALM)
Acral lentiginous melanoma accounts for approximately 2 to 8% of melanoma cases. It occurs on the palms, soles, nail beds and mucous membranes.
In the early stages, it appears as a flat, mottled, irregularly pigmented lesion. The lesion may be covered by hyperkeratosis. It is thus masked.
Under the nail, it resembles haemorrhagic changes. On the feet, it can be mistaken for a melanocytic nevus, lesion, blister or wart. Acral localised melanomas are often forgotten. Unfortunately, they are often diagnosed late.
subungual malignant melanoma Subungual malignant melanoma affects the nail bed. It is often diagnosed late. In most cases, it is treated as onychomycosis. In some cases, it is misdiagnosed as subungual bleeding after an accident (small shoes, tripping).
What are the other variants of malignant melanoma?
Amelanotic malignant melanoma (AMM)
Its diagnosis is very difficult. This type of melanoma is more aggressive than pigmented tumors. The prognosis is poor.
desmoplastic malignant melanoma It is very rare and difficult to diagnose. Pigment is often absent.
malignant melanoma in pregnancy In pregnancy, there is an increased production of hormones. The hormones stimulate the melanocytes to produce pigment. Darkening of pigmented lesions occurs. Sometimes, pre-existing malignant lesions are accentuated.
Pregnancy does not affect the survival of patients diagnosed with melanoma or the course of the disease. Patients do not have to worry about an increased risk of lymph node metastasis.
What does malignant melanoma look like?
Malignant melanoma is characterized by:
- Size - The tumor is usually larger than 6 mm, spreading and covering an increasingly larger area.
- Shape - The regular margin curls and develops protrusions or indentations.
- Colour - Darkening to blackening is most common.
- Surface - Scales, erosions and crusts form.
Diagnostics
Diagnosis of the disease is very important. When melanoma is diagnosed at an early stage, the prognosis of the disease is usually favourable.
When diagnosing malignant melanoma, we must first focus on the medical history, which focuses on:
- the presence of melanoma
- the method of tanning
- information on repeated sun exposure
- sunbathing in a tanning bed
- invasive procedure performed in the affected area
In the next step, it is important to assess the shape and size of the lesion. Subsequently, a palpation examination of the lymph nodes is performed. The doctor checks the skin capillaries, palms, soles, nails and mucous membranes.
For visual differential diagnosis, the ABCDE algorithm is most often used:
A (asymmetry) - asymmetry of the lesion
B (border irregularity) - border irregularity
C (color variegation) - uneven coloration
D (diameter) - size over 6 mm
E (evolution) - development, elevation of the lesion
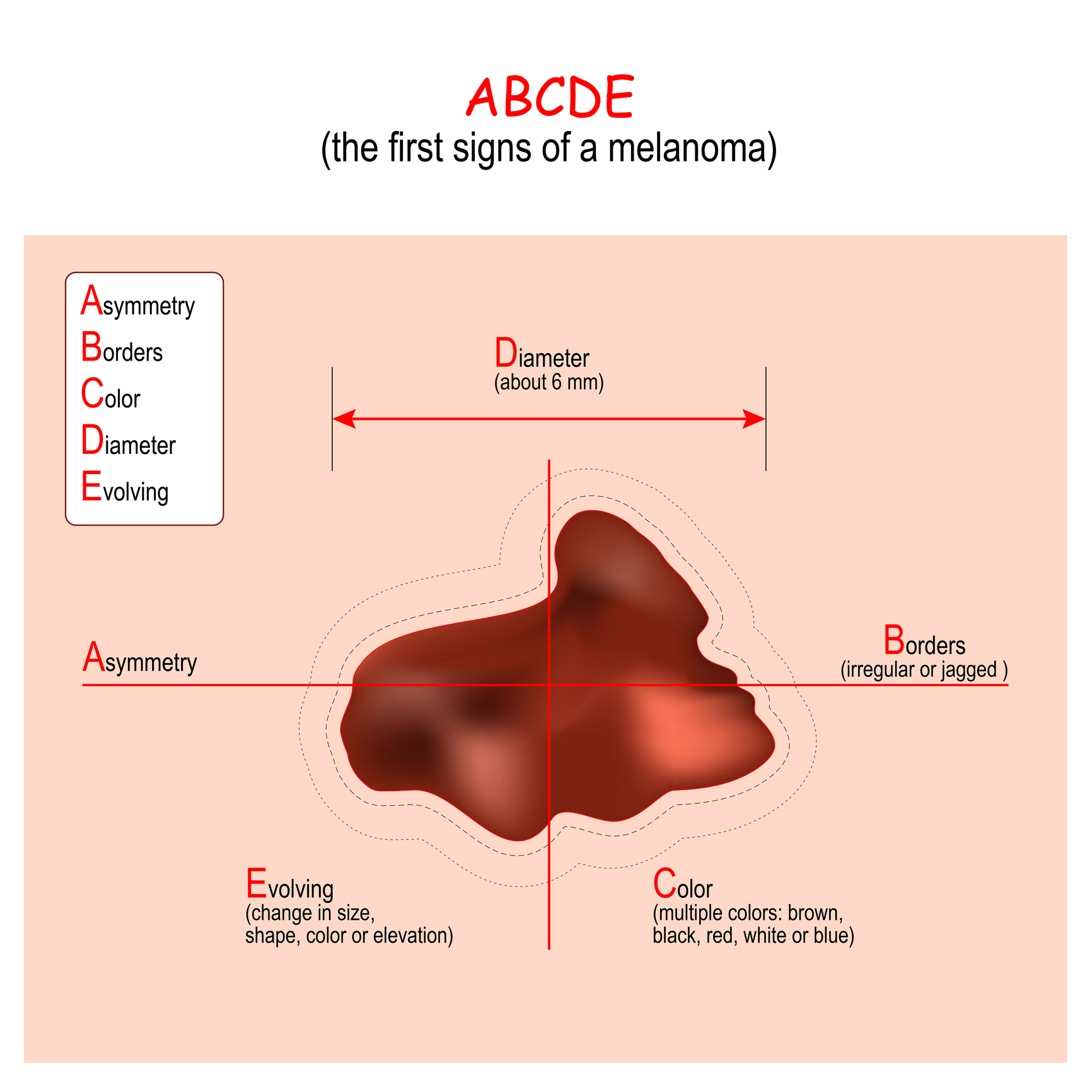
The ABCDE algorithm has several imperfections. In some situations, such as small lesions, it is inadequate.
To improve diagnosis, the 'ugly duckling' rule is still recommended. Every individual has a similar type of mole. They are similar clinically and histologically.
A nevus is a circumscribed skin formation that usually results from an embryonal developmental disorder.
In order to confirm the exact stage of the disease, we need to know the full extent of the disease. For this reason, sentinel node examination has been introduced into practice.
Sentinel lymphadenectomy is used for the early detection of clinically undetectable metastases. It is a diagnostic operation. Its aim is to catch nodal metastases at a clinically undetectable stage.
Sentinel node status is considered a major prognostic factor. It is crucial for the indication of adjuvant systemic therapy.
What is a sentinel node?
The sentinel node is the first place where cancer cells from the primary tumour reach via the lymphatic system.
What is the diagnosis of melanoma in children?
Melanoma in children is usually amelanotic, regular, monochromatic and less than 6 mm in size. The modified ABCD algorithm is used.
A (amelanotic)
B (bleeding, bump)
C (colour uniformity)
D (de novo development, any diameter) - newly formed, regardless of size
Dermatoscopy
In practice, a hand-held dermatoscope is most commonly used. This examination method uses a tenfold magnification of the lesion.
Thanks to the magnification, the physician can better determine the arrangement of pigment in the melanocytic formations, the behavior of the capillaries and detect the presence of inflammatory manifestations. The main goal of dermatoscopic examination is to distinguish:
- melanocytic lesions from non-melanocytic lesions
- benign lesions from malignant lesions
Currently, the method of digital dermatoscopy is used. This examination makes it possible to preserve the dermatoscopic image, to review it and to compare changes over time. Pigmentation is assessed by mathematical analysis.

Whole body scanning
One of the newest diagnostic methods is whole-body scanning. It is a non-invasive method used mainly in patients at high risk of developing malignant melanoma.
Interest in this examination is also growing among non-risk patients.
What is the aim of this method?
The main aim of the examination is to detect new or markedly macroscopically altered melanocyte manifestations in the skin. This examination method is only meaningful in repeated patient examinations because it tracks changes over time.
Histological diagnosis of melanoma
Any suspicion of melanoma should be an indication for surgical removal and histological diagnosis. Histological examination is the key to diagnosis.
The result of the histopathological examination of the removed tumour must include a macroscopic description of the lesion, which includes:
- length
- width
- thickness
- presence of haemorrhage
- crusts
- symmetry
- colouration
- localization
The histological picture varies according to the different types of melanoma. In general, there are common features of the malignant nature of the lesion.
These features include asymmetry in the outline and arrangement of the lesion, blurred edges or the formation of irregular nests of tumour cells of different sizes.
The basic requirements for histological examination of melanoma include:
- tumour thickness in mm (Breslow value)
- number of mitoses per 1 mm2 for tumours less than 1 mm thick
- assessment of the presence/absence of ulceration
- assessment of the presence/absence of regression
- width of the safety margin
Course
The course and prognosis of the disease depends on the development of the primary tumour.
The basic histopathological parameters for learning the severity of melanoma include:
- tumor thickness - also referred to as Breslow value
- depth of invasion - assesses the depth to which the tumour has penetrated
- superficial ulceration - occurs spontaneously
- mitotic index - number of mitoses per 1 mm2
- sentinel node status - metastases in this node significantly worsen the prognosis of the disease
In practice, two phases of tumour growth are distinguished:
- Horizontal-radial growth phase - Atypical melanocytes penetrate into the higher layers of the epidermis and epidermal areas distant from the site of primary melanocyte proliferation. Clones with different growth and melanin production rates are formed.
- Vertical growth phase - Cells from one of the clones penetrate the mosaic and continue to proliferate. Biologically adverse tumour characteristics are associated with vertical growth.
Clark et al. introduced a prognostic-histological classification based on the degree of invasion:
- Stage I invasion - Tumor cells are only in the epidermis above the basement membrane.
- Stage II invasion - Tumor cells penetrate the basement membrane into the stratum papillare.
- Stage III invasion - Tumor cells reach the boundary between the stratum papillare and stratum reticulare.
- Stage IV invasion - Tumour cells penetrate between collagen fibres.
- V stage of invasion - Tumour cells penetrate below the dermal adipose tissue.
The dermis consists of:
- Stratum reticulare - loose confinement with the subcutaneous tissue, dense collagenous connective tissue
- Stratum papillare - clear, wavy border with the epidermis, sparse collagenous connective tissue
How it is treated: Malignant melanoma
How is malignant melanoma treated? Surgery - surgery and drugs
Show moreMalignant melanoma is treated by
Other names
Interesting resources
Related










