- solen.sk - Posttraumatic hydrocephalus, MUDr. Lubomír Jurák, Ph.D., doc. MUDr. Vladimír Beneš, Ph.D., III, prof. MUDr. Petr Suchomel, Ph.D., Neurocentrum, Regional Hospital Liberec, a.s.
- Solen.sk - Hydrocephalus, prof. MUDr. Martin Smrčka, Ph.D., MBA - editor of the main topic, Department of Neurosurgery, Faculty of Medicine, Brno.
- solen.sk - Normotensive hydrocephalus, Václav Vybíhal, M.D., Department of Neurosurgery, Faculty of Medicine, Medical University of Brno.
- ncbi.nlm.nih.gov - Hydrocephalus
- pubmed.ncbi.nlm.nih.gov - Hydrocephalus
- mayoclinic.org - Hydrocephalus Mayoclinic
Hydrocephalus: What is it and why does it occur? What are the symptoms and consequences?

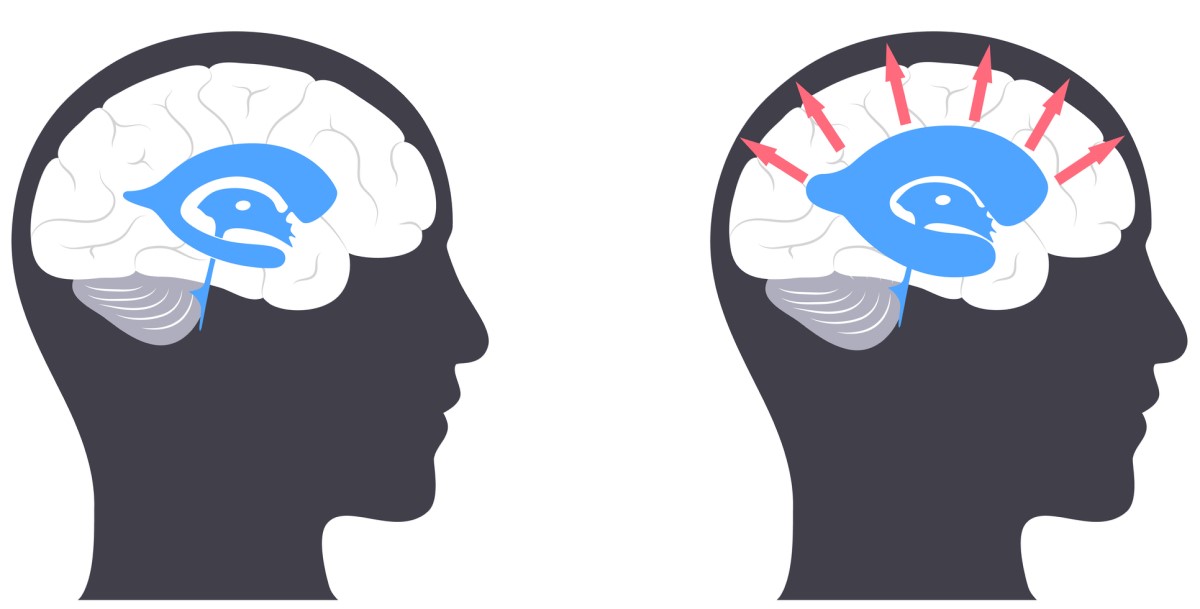
Hydrocephalus is a disease that mainly affects newborns and the elderly. It is an increased amount of cerebrospinal fluid in the ventricles of the brain. The increased volume of fluid increases intracranial pressure, causing a number of characteristic symptoms. Diagnosis is rapid, using modern imaging tests. Treatment is so far only surgical.
Most common symptoms
Characteristics
Because all fluid is incompressible, when it accumulates in this hard shell, pressure builds up rapidly, adversely affecting the soft and fragmented brain tissue.
Increasing pressure in the skull and pressure on brain structures is the cause of the symptoms of hydrocephalus, which can have fatal consequences.
Cerebrospinal fluid (liquor) forms in the so-called plexus chorioideus (chorioid plexus). This is a densely vascularised tissue formed by the interstitial pia mater - the soft brain membrane that covers the surface of the brain.
The chorioid plexus is located on the ceiling of all four ventricles of the brain. It is found in the lateral ventricles (I and II), which are located in the hemispheres. It is also found in the third ventricle, which is located in the midbrain region, and in the fourth and final ventricle, which is located behind the brainstem and the medulla oblongata and is surrounded by the cerebellum.
The fluid flows from the lateral hemispheric ventricles into the third ventricle through an opening called the orifice of Monroe. From the third ventricle it flows through the aqueduct of Sylvius into the fourth ventricle.
From there, it enters the subarachnoid spaces through three other openings. It is then absorbed into the venous sinuses and from there, along with the venous blood, is drained out of the skull towards the heart.
Circulation of the flowing fluid is ensured by the rhythmic cardiac cycle. During cardiac systole, the compression of the ventricles, the fluid is forced down into the spinal canal.
During diastole, or cardiac relaxation, fluid flows upward into the brain.
Each person normally produces approximately 500 ml of cerebrospinal fluid per day.
The total volume of fluid in the ventricles of the brain and around the spinal cord is between 80 and 150 ml. This means that all the fluid is completely replenished three times in 24 hours.
Causes
There are three basic types of hydrocephalus depending on the level at which the circulatory system is disturbed.
Communicating hydrocephalus
This type of hydrocephalus is characterized by the absence of any obstruction in the ventricular system. Hence the name communicating. It is caused by either increased production or, conversely, decreased absorption of liquor.
- Hypersecretory hydrocephalus is a relatively rare type of hydrocephalus. Increased production of liquor may be caused, for example, by tumour spread in the plexus chorioideus, which is the main organ of liquor production. The most common tumours affecting the plexus are papilloma or carcinoma. Hypersecretory hydrocephalus may also occur in non-tumoural disease of the plexus, e.g. plexus hypertrophy, i.e. benign enlargement of the plexus chorioideus tissue.
- Hyporesorptive hydrocephalus is the most common type of hydrocephalus. It is caused by a defect in the absorption of fluid, which can arise for many reasons.
The most common causes include sclerotization (hardening and malfunction) of the arachnoid granulations that are located on the surface of the cerebral hemispheres.
This process occurs after overcoming meningitis, after bleeding into the subarachnoid space, as a result of trauma with disruption of the dura mater (hard shell of the brain) or after neurosurgical intervention, e.g. after decompressive craniectomy.
Other possible causes are thrombosis of the venous plexus or stenosis (narrowing) of the foramen jugulare (the opening in the skull through which the jugular vein and the three cranial nerves pass) with subsequent venous hypertension.
Obstructive hydrocephalus
This type of hydrocephalus results from an obstruction in the circulation of the liquor. This obstruction may be located anywhere in the course of the liquor pathways, but most commonly in the region of the aqueduct of Sylvius.
The cause of the obstruction may be, for example, congenital narrowing of this site (stenosis), post-inflammatory changes (e.g. gliosis, i.e. replacement of functional tissue by glial cells - similar to a scar), haemorrhage or tumour.
Among tumours, germinoma, pinealocytoma or pinealoblastoma are the most common.
The second site where fluid flow is often obstructed is the ostium of Monroe. It is located in the third and fourth ventricles of the brain. At this site, the obstruction may be formed by cysts, such as a colloid or arachnoid cyst.
Not infrequently, it is also a neoplasm, e.g., brainstem glioma, medulloblastoma, or ependymoma.
Obstructive hydrocephalus also occurs after subarachnoid haemorrhage and is a serious complication of this life-threatening condition.
Specific types of hydrocephalus
- In normotensive hydrocephalus, there is an increased volume of fluid in the liquor ducts, but intracranial pressure does not increase. It affects mainly elderly people. It is characterised by a triad of symptoms: dementia or slowed psychomotor pace with memory impairment, difficulty in walking (a staggering gait called atactic gait), sphincter problems most commonly urinary incontinence.
- Pseudotumor cerebri is a disease that typically affects obese middle-aged women. It involves increased intracranial cerebrospinal fluid pressure. Symptoms include headaches and visual disturbances. However, memory impairment, disorientation and impaired mental function as in other types of hydrocephalus are absent. Treatment is surgical and consists of creating a drainage of the liquor outside the cranial cavity.
Hydrocephalus most commonly occurs in infancy as a result of many birth defects and also as a result of cerebral hemorrhage in premature infants.
The overall prevalence of hydrocephalus is approximately 85 cases per 100 000 population. However, children are more often affected, up to 88 per 100 000. The adult population is affected much less, 11 per 100 000.
A second peak in the prevalence of hydrocephalus follows in the elderly, with a prevalence of approximately 175 per 100 000 and more than 400 per 100 000 after the age of 80.
In terms of geographical differences, people in Africa and South America are most affected by hydrocephalus.
There is no significant difference between the sexes and both sexes can be affected equally.
Symptoms
Acute hydrocephalus
Acute closure of the liquor ducts leads to rapid dilatation of the lateral ventricles and an increase in intracranial pressure. Too much pressure will press on soft brain tissue, which will subsequently be forced out through the brain openings.
This situation is called brain herniation and is a life-threatening condition.
Warning signs are headache and vomiting with no prior nausea or relief from vomiting. This is followed by altered consciousness, dilated unresponsive pupils, and even coma with slowed heart rate.
Congenital hydrocephalus
Congenital hydrocephalus usually appears just after birth.
Typical symptoms are as follows:
- abnormally large head
- tense, bulging and minimally pulsating fontanelle
- splitting of the cranial sutures
- thin and shiny scalp
- accentuated venous pattern on the head
- stiff arms and legs
- eye pupils are close to the lower lid margin, giving the impression of a "setting sun"
- difficulty breathing
- lack of appetite and refusal of food
- reluctance to move the neck or turn the head
- delayed psychomotor development
Late onset of hydrocephalus
Slower-onset hydrocephalus is characterized by headaches and a typical triad of symptoms:
- Psychomotor retardation with memory impairment and developing dementia.
- Gait disturbance called ataxia. Gait is limp, uncoordinated, without balance and stability.
- Sphincter disorder manifested by incontinence, i.e. leakage of urine in varying degrees.
Diagnostics
In the case of acute hydrocephalus, CT (computed tomography) of the brain is the fastest and most accessible examination. With this examination, we can immediately assess the size of the brain ventricles.
Increased amounts of intracranial fluid will appear around the ventricles as 'periventricular preenhancement', i.e. darkening of the ventricular surroundings caused by leaking fluid under high pressure.
The second sign of hydrocephalus is an inflation of the anterior horns of the lateral hemispheric ventricles and the third ventricle. This sign is also referred to as "Mickey Mouse" because the image resembles the famous cartoon character.
The presence of this sign indicates an obstruction in the region of the aqueduct of Sylvius.
The best and most detailed examination is clearly a magnetic resonance imaging (MRI) of the brain.
It shows the structures of the posterior fossa very well and with its help we can distinguish between brain tumours and degenerative diseases and we can also distinguish normotensive hydrocephalus from cerebral atrophy.
On MRI images, increased cerebrospinal fluid volume is shown as periventricular hyperintensity (luminal deposits) in T2 sequences. These sequences are specifically used in the identification of fluid components in the brain.
Diagnosis is difficult in chronic (long-term) hydrocephalus. In this case, the anterior horns of the lateral ventricles may not be as markedly enlarged.
Some important centers in the brain may even be shrunken (atrophied), so that some neurodegenerative diseases must be ruled out.
The diagnostic test for normotensive hydrocephalus is the so-called TAP test. In this test, a lumbar puncture is carried out in which a large amount of fluid is drained, 30 to 50 ml. After a few hours, the patient is examined.
If there is a significant improvement in his symptoms, normotensive hydrocephalus is highly probable. The test is actually an external drainage from the liquor ducts.
For congenital forms of hydrocephalus, it is recommended to undergo genetic testing and counselling in case of further pregnancy.
In newborns, the simplest method of examining the brain is ultrasonography (USG), where the probe of the machine is placed on the surface of the cerebellum - the anterior greater fontanelle.
The examination does not load the baby's small body with radiation and it is not necessary for the baby to be at rest, as is the case with MRI. Therefore, ultrasound can be performed more frequently and is also useful for monitoring the progression of hydrocephalus or the effectiveness of therapy.
Dopplerometry is a function of ultrasonography in which we can monitor changes in cerebral perfusion. We can thus assess the degree of intracranial hypertension and the functionality of drainage (hydrocephalus therapy).
An ophthalmologist can also diagnose increased intracranial pressure. When examining the background of the eye, he or she will notice edema (swelling) of the optic nerve papilla. The optic nerve papilla is where the optic nerve leaves the retina and continues on to the brain.
This symptom clearly indicates increased pressure in the skull, which can be caused by a tumor or even hydrocephalus.
Course
In acute hydrocephalus, the obstruction in the liquor system arises suddenly, and the condition progresses very quickly.
The patient has severe symptoms of increased intraluminal pressure, which include mainly an unremitting headache and vomiting with no previous nausea. There is no relief after vomiting, as there is, for example, in gastric upset.
The patient may quickly fall unconscious, convulsions, disorientation and even coma may occur.
An acute CT scan of the brain and neurosurgical intervention to relieve the mounting pressure in the skull should be performed immediately.
The greatest risk in acute hydrocephalus is brain herniation, i.e., the displacement of brain tissue through one of the openings in the skull. This condition can end in failure of vital signs and sudden death.
In chronic hydrocephalus, which develops over a longer period of time, the symptoms are not as dramatic. Its progression is less noticeable. One type of chronic hydrocephalus is normotensive hydrocephalus. It mainly affects the elderly.
The main symptom is a slowing of the psychomotor pace, which is reminiscent of incipient dementia. Urinary incontinence and even complete bed-wetting are associated. Because these symptoms also occur in other diseases associated with old age, normotensive hydrocephalus often escapes proper diagnosis.
The patient is often investigated at length for the presence of neurodegenerative diseases. With gait disturbance that is ataxic (unsteady) with impaired balance and stability, the diagnosis may be mistaken for Parkinson's disease.
A special MRI scan with flow measurement in the liquor pathways and the so-called TAP test will reveal the real cause of the difficulty and treatment will relieve the patient's symptoms to a high degree.
In the case of congenital hydrocephalus, the diagnosis is often already known at birth. The congenital brain development defect that causes hydrocephalus can be diagnosed during pregnancy.
The child has an enlarged head circumference, split intercranial sutures, a non-pulsatile fontanelle and a prominent venous pattern on the head. He is restless, refuses to suck from the breast, is tearful, does not move his neck or turn his head.
The therapy is the same as in adulthood, namely the insertion of a drainage system. After the operation, the child leads a normal life, the drain does not need to restrict him in any way. Increased attention should be paid to the pressure setting on the valve and the risk of infection.
How it is treated: Hydrocephalus
Treatment of hydrocephalus: Medication? Surgery, drainage required
Show moreHydrocephalus is treated by
Other names
Interesting resources










